Urethral Reconstruction: What It Means and Why It Matters
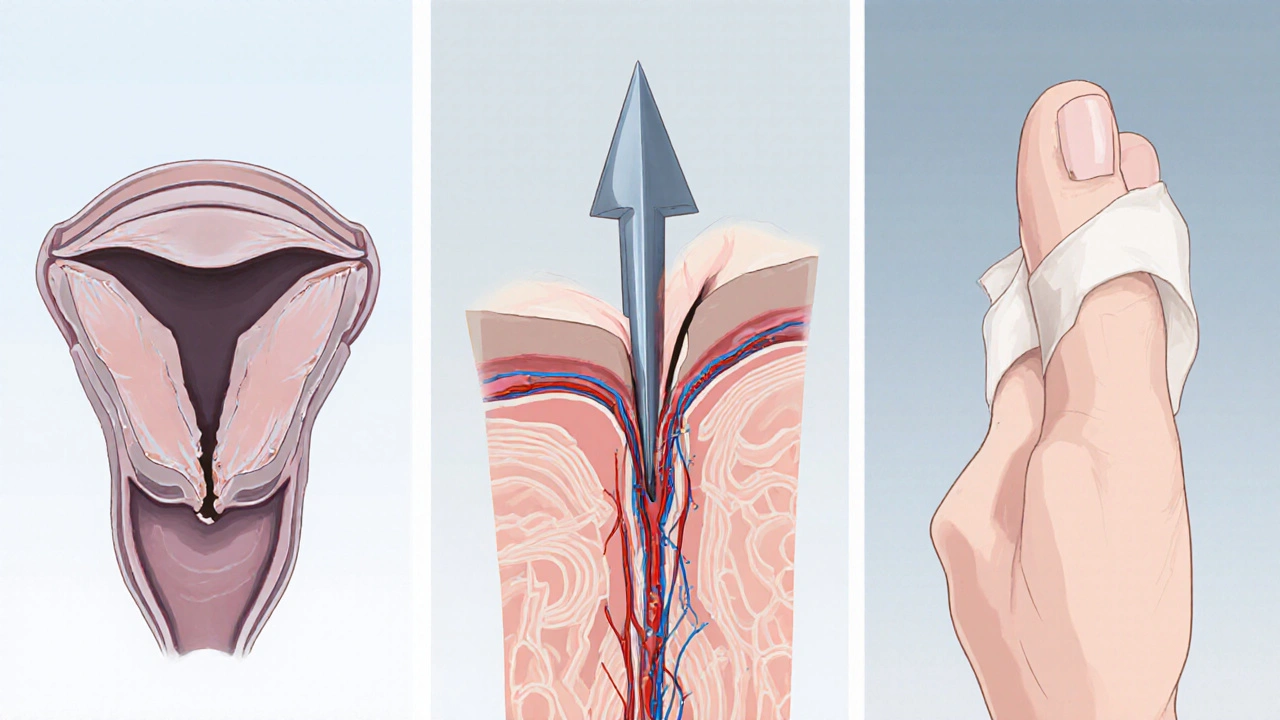
When dealing with urethral reconstruction, the surgical repair of the urethra to restore normal urine flow. Also known as urethroplasty, surgeons often address a urethral stricture, a narrowing that blocks urine by using a tissue graft, a piece of skin or buccal mucosa to rebuild the pipe. When the condition results from pelvic trauma, injury that damages the pelvic floor and urethra, reconstruction becomes essential. In short, urethral reconstruction encompasses urethral stricture repair, requires tissue grafts for long gaps, and is heavily influenced by the severity of pelvic trauma.
Key Considerations for Successful Urethral Reconstruction
The first step is a thorough diagnosis – imaging, endoscopy, and urodynamic tests help map the exact length and location of the defect. Surgeons then choose a technique that matches the gap size: a simple excision and primary anastomosis works for short segments, while longer gaps need a tissue graft or flap. Buccal mucosa grafts are popular because they resist infection and integrate well, whereas skin grafts are reserved for very large reconstructions. The choice of graft influences both operative time and postoperative outcomes, making graft selection a pivotal decision. Once the graft is in place, a supportive stent may stay for a few weeks to keep the new channel open, reducing the risk of re‑stricture.
Recovery focuses on protecting the repair while the tissue heals. Patients are usually advised to avoid heavy lifting, vigorous activity, and sexual intercourse for six to eight weeks. A short course of antibiotics prevents infection, and regular follow‑up cystoscopies catch early signs of narrowing. Complications can include bleeding, infection, or a new stricture, but modern techniques report success rates above 80 % for appropriately selected cases. Understanding how pelvic trauma adds complexity – often requiring a combined urologic‑vascular approach – helps set realistic expectations and guides postoperative care.
Below you’ll find articles that dive deeper into each aspect of urethral reconstruction, from graft options and surgical tips to patient‑focused recovery strategies. Whether you’re a caregiver, a medical professional, or someone facing this surgery, the collection offers practical insights you can act on right away.
Penile Reconstructive Surgery: How It Repairs Traumatic Injuries
Learn how penile reconstructive surgery restores function and appearance after trauma, with clear explanations of techniques, recovery, risks, and how to choose a specialist.
