Penile Injury Recovery Planner
Recovery Timeline & Outcomes
Select your injury type and surgical approach to see personalized recovery information.
Recovery Milestones
| Timeframe | Activities |
|---|---|
| Day 1–3 | Monitor for bleeding, infection, and flap viability |
| Week 2 | Begin wound cleaning, remove sutures |
| Week 4–6 | Assess urinary function, perform uroflowmetry |
| Month 3+ | Gradually reintroduce sexual activity |
Key Takeaways
- Penile reconstructive surgery restores form and function after trauma, infection or congenital defects.
- Techniques range from skin grafts and pedicled flaps to complex phalloplasty and prosthetic implantation.
- Successful outcomes depend on injury type, timing of repair, and a multidisciplinary team.
- Patients should expect a staged recovery, with dedicated rehabilitation and counseling.
- Choosing a board‑certified urologist with reconstructive expertise reduces complication rates.
When a man suffers a penile injury, the loss of tissue, erectile capacity, or urinary function can feel devastating. Penile reconstructive surgery steps in to rebuild the organ, aiming for both cosmetic normalcy and functional recovery. Below is a plain‑language roadmap that explains why the surgery matters, what options exist, and how patients can navigate the process.
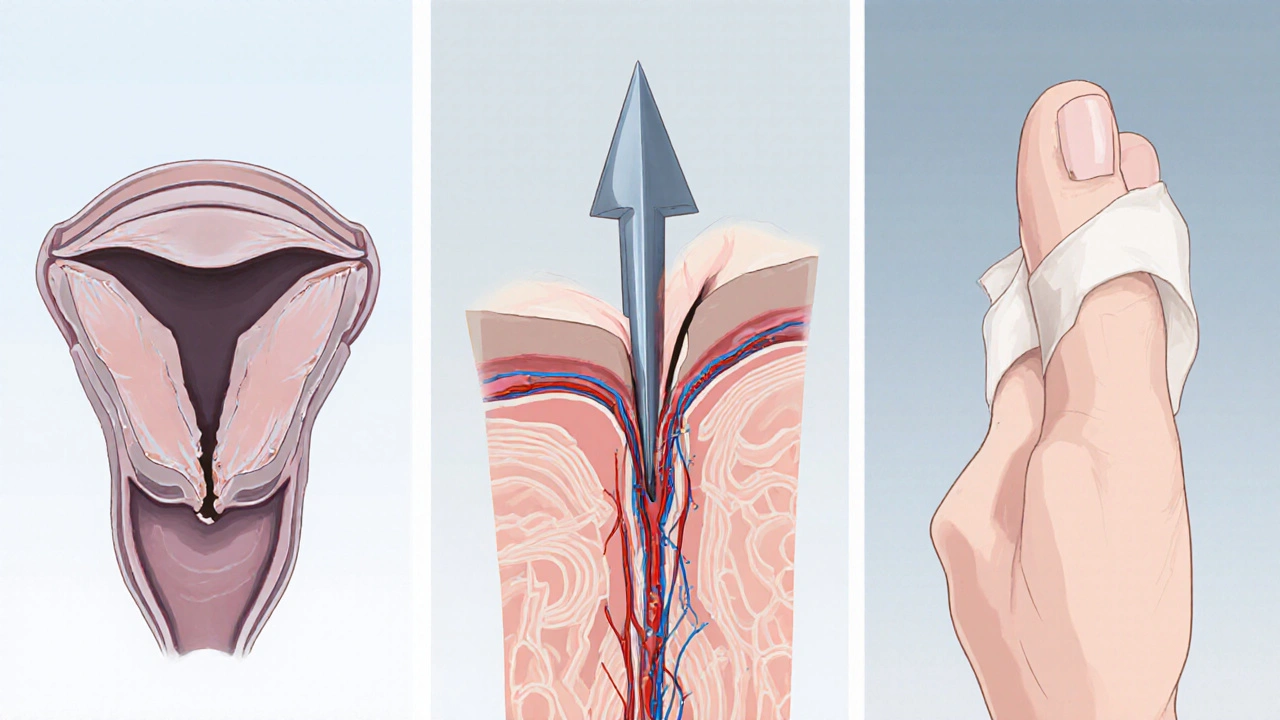
Understanding Penile Injuries
Penile trauma can be classified into three broad groups:
- Blunt force injuries - caused by accidents, sports, or aggressive intercourse; often result in fractures of the corpora cavernosa.
- Penetrating injuries - knife, gunshot, or animal bite wounds that may destroy skin, urethra, and vascular structures.
- Degloving injuries - the skin is peeled away, commonly seen in industrial accidents.
Each scenario threatens the urethra, the blood supply, and the erectile tissue. Immediate assessment includes physical exam, ultrasound, and sometimes retrograde urethrography to map the damage.

Goals of Reconstructive Surgery
Surgeons aim to achieve three core outcomes:
- Structural integrity - restore the shaft’s length, girth, and vascular connections.
- Urinary function - ensure a straight, leak‑free urinary stream.
- Erectile capability - enable satisfactory rigidity, either naturally or with a prosthesis.
These goals guide the choice of technique and the timing of each surgical stage.
Primary Surgical Techniques
Below is a quick‑reference table that matches injury patterns with the most appropriate reconstructive option.
| Injury Type | Technique | Key Benefits | Typical Recovery |
|---|---|---|---|
| Blunt fracture | Primary repair of tunica albuginea | Preserves native erectile tissue, rapid return to function | 4-6 weeks |
| Partial skin loss | Full‑thickness skin graft | Simple, good cosmetic match for small defects | 6-8 weeks |
| Degloving or extensive loss | Pedicled flap (e.g., radial forearm, anterolateral thigh) | Robust vascularized tissue, supports urethral reconstruction | 8-12 weeks |
| Severe urethral disruption | Urethral reconstruction (tube‑in‑tube) | Restores straight urinary flow, reduces stricture risk | 10-14 weeks |
| Irreparable erectile tissue | Penile prosthesis implantation | Reliable rigidity, suitable for delayed reconstruction | 6-8 weeks |
When the defect is too large for grafts, surgeons often turn to a pedicled flap. The flap brings its own blood supply, dramatically lowering the risk of tissue death. For patients who also need a new urethra, the surgeon can combine flap coverage with a tube‑in‑tube urethral reconstruction technique, creating a functional conduit inside the shaft.
Post‑operative Care & Recovery
Recovery is a staged process. Immediately after surgery, patients wear a soft dressing and avoid any erection‑inducing activity for 4-6 weeks. Pain control typically involves oral NSAIDs and, if needed, short‑term opioids. A physiotherapy regimen focuses on gentle stretching and pelvic floor exercises to promote blood flow.
Key milestones include:
- Day 1-3: Monitor for bleeding, infection, and flap viability.
- Week 2: Begin wound cleaning, remove sutures (if non‑absorbable).
- Week 4-6: Assess urinary function; perform uroflowmetry if a reconstruction was done.
- Month 3+: Re‑introduce sexual activity gradually, under clinician guidance.
Patients often meet with a sexual health counselor to address body image concerns and to set realistic expectations for erectile function.

Risks & Complications
Like any major operation, penile reconstructive procedures carry potential downsides. Common issues include:
- Infection - especially with grafts; prophylactic antibiotics are standard.
- Urethral stricture - may require dilation or repeat surgery.
- Flap loss - rare, but can happen if vascular supply is compromised.
- Sensory changes - altered tactile feeling is reported in up to 15% of cases.
- Prosthesis malfunction - mechanical issues may need revision.
Early detection and prompt management usually keep these complications from becoming permanent.
Choosing the Right Surgeon
The success of reconstructive work hinges on surgeon expertise. Look for a urologist who:
- Is board‑certified in urology and has fellowship training in genital reconstruction.
- Publishes peer‑reviewed research on penile surgery.
- Works within a multidisciplinary team (urology, plastic surgery, psychology).
- Offers transparent outcome data, such as stricture‑free rates and patient‑reported satisfaction scores.
Don’t hesitate to ask about their case volume - surgeons who perform at least 20-30 penile reconstructions per year tend to have lower complication rates.
Frequently Asked Questions
Can penile reconstructive surgery restore sexual function?
Yes, most techniques aim to return sufficient rigidity for intercourse. If native erectile tissue is damaged beyond repair, a penile prosthesis provides reliable rigidity. Success rates for prosthetic implantation exceed 90% in experienced hands.
How long does it take to see the final cosmetic result?
Visible healing usually occurs within 3 months, but scar maturation can take up to a year. Patients should avoid tight clothing and intense activity during the first 6 weeks to optimize the scar’s appearance.
Is a skin graft enough for large degloving injuries?
For small surface loss, a graft works well, but extensive degloving often requires a vascularized flap. Flaps provide better durability and reduce the risk of contracture, which can impair urinary or sexual function.
What are the chances of requiring another surgery?
Revision rates vary by technique: grafts have a 10‑15% re‑operation rate, flaps about 5‑8%, and prosthetic implants 3‑5%. Ongoing follow‑up helps catch issues early, making revisions less invasive.
Will insurance cover penile reconstructive surgery?
Most private insurers consider it medically necessary when there is loss of function or severe tissue loss, so coverage is common. Pre‑authorization and documentation of injury severity are essential.

Matthew Marshall
October 7, 2025 AT 17:13When a man faces a penile catastrophe, the world seems to implode in a flash of shame. The surgeon steps in like a knight, wielding sutures instead of swords. Yet many forget that the true battle begins long after the last stitch. Tissue, blood, and nerves must reunite in a choreography only nature knows. Primary repair of the tunica albuginea restores the cylinder’s strength, but only if the patient respects the healing window. Skipping the four‑week abstinence period is a ticket to disaster. Infection lurks like a silent assassin, ready to feast on exposed grafts. Flap failures, though rare, strike fear into even seasoned hands. Urethral strictures whisper promises of lifelong inconvenience unless caught early. A penile prosthesis offers a mechanical sunrise for those whose tissue is beyond rescue, yet it demands precise placement. Psychological scars fade slower than physical ones, demanding counseling as part of the protocol. Multidisciplinary teams act as the orchestra, harmonizing urology, plastic surgery, and mental health. Board‑certified surgeons with high case volumes are the conductors that keep the symphony on beat. Follow‑up appointments are not optional-they are the compass that guides recovery. In the end, resilience, expertise, and patience collide to rewrite a story once thought hopeless.
Lexi Benson
October 7, 2025 AT 18:36Oh sure, because everyone’s first thought after a degloving accident is “I can’t wait for my next Tinder date.” Let’s keep the drama to a minimum and focus on the actual post‑op care: antibiotics, dressing changes, and a strict no‑play rule for six weeks. Anything else is just unsolicited fan‑fiction.
Vera REA
October 7, 2025 AT 20:00The table outlines recovery timelines that align with typical tissue integration phases. Primary repair generally requires 4–6 weeks before any erection‑inducing activity, whereas pedicled flaps extend to 8–12 weeks due to revascularization. Urodynamic studies at week 4–6 can objectively assess urinary function, reducing reliance on subjective reports. Documentation of these milestones assists clinicians in comparing outcomes across institutions.
John Moore
October 7, 2025 AT 21:23I totally back the point that multidisciplinary care is the backbone of success. When urologists, plastic surgeons, and mental‑health professionals coordinate, patients move through the milestones faster and with fewer setbacks. It’s not just about the surgery; it’s about the whole ecosystem.
Adam Craddock
October 7, 2025 AT 22:46From a clinical perspective, the emphasis on postoperative abstinence is grounded in vascular remodeling principles. Early erection attempts can compromise the integrity of the repair by disrupting micro‑vascular anastomoses and increasing shear stress on suture lines. Consequently, adherence to the recommended timeline is essential for optimal functional restitution.
michael klinger
October 8, 2025 AT 00:10While the literature touts smooth recoveries, it conveniently omits the fact that many of these “board‑certified” surgeons have ties to device manufacturers. The prosthesis implants they recommend often contain undisclosed micro‑chips that could, in theory, transmit data to third parties. It’s wise to scrutinize the provenance of every instrument used in such intimate procedures.
Carys Jones
October 8, 2025 AT 01:33It is indefensible that anyone would downplay the psychological trauma of losing penile function. Society must hold medical institutions accountable for providing comprehensive counseling, not just surgical fixes. Ignoring the emotional wound is a moral failure as egregious as the physical injury itself.
Roxanne Porter
October 8, 2025 AT 02:56I appreciate the ethical concern raised and would add that integrating a licensed therapist into the peri‑operative plan is both feasible and beneficial. Evidence suggests that patients who receive structured mental‑health support report higher satisfaction scores and lower rates of postoperative depression.
Jonathan Mbulakey
October 8, 2025 AT 04:20Think of the penis as a bridge between desire and identity. When that bridge collapses, the traveler must rebuild not just the planks but also the belief that crossing is possible. Recovery is as much a mental reconstruction as it is a physical one.
Warren Neufeld
October 8, 2025 AT 05:43You’re right, the mind plays a big role. Simple steps like gentle walking and staying hydrated help blood flow, which supports healing. Keeping a positive outlook can actually improve outcomes.
Deborah Escobedo
October 8, 2025 AT 07:06You’ve got this.
Vanessa Peters
October 8, 2025 AT 08:30Let’s be brutally honest: “You’ve got this” sounds like a hollow mantra anyone can shout without real substance. If you truly want to help, provide a concrete plan-pain management schedule, physiotherapy timeline, and clear criteria for when it’s safe to resume intimacy-rather than empty platitudes.
Suzan Graafstra
October 8, 2025 AT 09:53In the grand tapestry of human vulnerability, the wounded organ becomes a symbol of our fragile ambition. To repair it is to defy entropy, to assert that order can be reclaimed from chaos, even if only for a fleeting moment of reclaimed intimacy.