Population Pharmacokinetics: How Drugs Work Differently in Real People
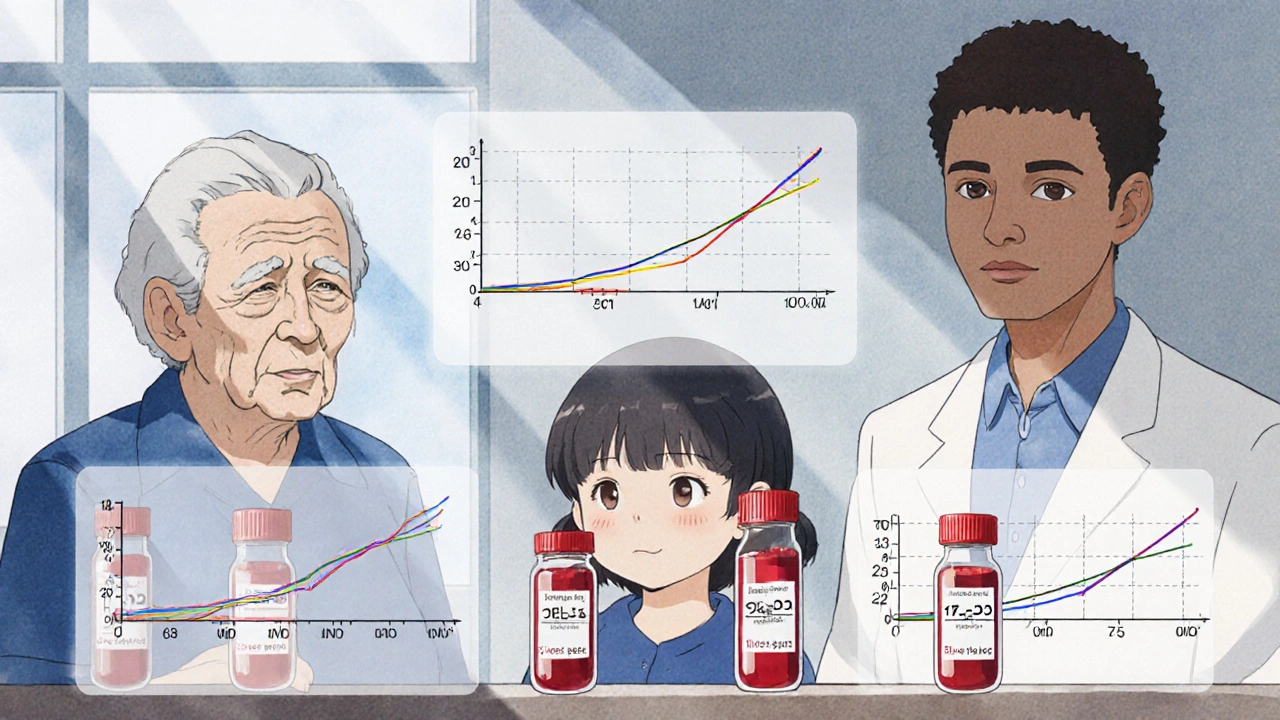
When you take a pill, it doesn’t behave the same way in everyone. Population pharmacokinetics, the study of how drug absorption, distribution, metabolism, and elimination vary across groups of people. Also known as popPK, it’s the science behind why a 70mg dose of a drug might help one person and harm another. This isn’t about mistakes or bad prescriptions—it’s about biology. Your age, weight, liver function, kidney health, even your genes, change how your body handles medicine. Population pharmacokinetics looks at these patterns across hundreds or thousands of people to predict what works best for whom.
It’s not just theory. Doctors and pharmacists use it every day to avoid dangerous side effects. For example, older adults often process drugs slower, so they need lower doses. People with kidney disease may build up toxic levels of certain medications if dosing isn’t adjusted. Drug metabolism, how the body breaks down medications using enzymes like CYP450, varies wildly between individuals. Some people are fast metabolizers—drugs leave their system too quickly to work. Others are slow, and even small doses can cause overdose. Individualized dosing, tailoring medicine amounts based on patient-specific factors is the goal. It’s why pharmacists ask about your other meds, your diet, and your health history before filling a prescription. They’re not just being thorough—they’re using popPK principles to keep you safe.
This field connects directly to real-world issues you’ll find in the articles below. From understanding why proton pump inhibitors cause long-term problems in some but not others, to knowing why antidepressants can trigger mania in people with bipolar disorder, it’s all tied to how drugs move through different bodies. Pharmacokinetic modeling, mathematical tools that predict drug behavior based on patient data helps explain why some people need higher doses of finasteride for hair loss, or why benzodiazepines are riskier when mixed with opioids in older adults. It’s also why telepharmacy and automated dispensing cabinets now include popPK-based alerts—to catch dangerous interactions before they happen.
You’ll find articles here that don’t just talk about drugs—they show how they behave in real people. Whether it’s why naloxone works fast in opioid overdoses, how oral corticosteroids harm bones over time, or why feverfew increases bleeding risk with blood thinners, each post ties back to one truth: medicine isn’t one-size-fits-all. The articles below give you the tools to understand your own body’s response to drugs, spot potential risks, and ask the right questions. You’re not just reading about medications—you’re learning how to make them work for you, not against you.
Population Pharmacokinetics: How Data Proves Drug Equivalence Beyond Traditional Bioequivalence Studies
Population pharmacokinetics uses real-world patient data to prove drug equivalence across diverse populations, offering a more accurate and ethical alternative to traditional bioequivalence studies.
