When two drugs are supposed to do the same thing, how do you prove they work the same way in real patients-not just in healthy volunteers? Traditional bioequivalence studies have long relied on small groups of healthy people, taking multiple blood samples over hours, to compare drug levels. But what if the drug is meant for elderly patients with kidney problems, or children, or people on multiple medications? Those groups rarely show up in those classic studies. That’s where population pharmacokinetics comes in.
What Population Pharmacokinetics Actually Does
Population pharmacokinetics, or PopPK, isn’t about finding the average drug level in a perfect lab setting. It’s about understanding how drug concentrations change across real people with real differences-age, weight, liver function, genetics, other drugs they’re taking. Instead of needing 8-10 blood draws per person, PopPK works with just 2 or 3 samples per patient, collected during normal clinic visits. That’s the game-changer.This approach uses advanced math called nonlinear mixed-effects modeling. Think of it like building a statistical profile of a drug’s behavior across hundreds of patients at once. The model pulls out patterns: maybe people with low kidney function clear the drug 40% slower. Or maybe heavier patients need a higher dose to hit the same blood level. It doesn’t just say ‘the average is the same.’ It tells you whether the variability between two versions of the drug is small enough to be safe.
Before PopPK, proving equivalence in special populations often meant running separate, expensive, and sometimes unethical trials. Now, with enough real-world data, regulators can say: ‘We don’t need another trial. The model shows these two formulations deliver the same exposure across the whole group.’
Why Regulators Are Now Accepting PopPK
The U.S. Food and Drug Administration (FDA) made a major shift in February 2022. For the first time, they published formal guidance saying PopPK data can replace some post-marketing studies. That’s huge. It means companies can use existing clinical trial data-not just lab-based bioequivalence studies-to prove their generic or biosimilar drug works just like the brand-name version.The European Medicines Agency (EMA) has been on board since 2014, emphasizing that PopPK can account for patient characteristics like age or organ function. Japan’s PMDA followed in 2020. This isn’t a fringe idea anymore-it’s becoming standard for complex drugs.
Why now? Because the data speaks. Between 2017 and 2021, about 70% of new drug applications to the FDA included PopPK analyses. Companies like Pfizer and Merck have shown that using PopPK reduced the need for extra clinical trials by 25-40%. That saves millions and gets life-saving drugs to patients faster.
How PopPK Beats Traditional Bioequivalence
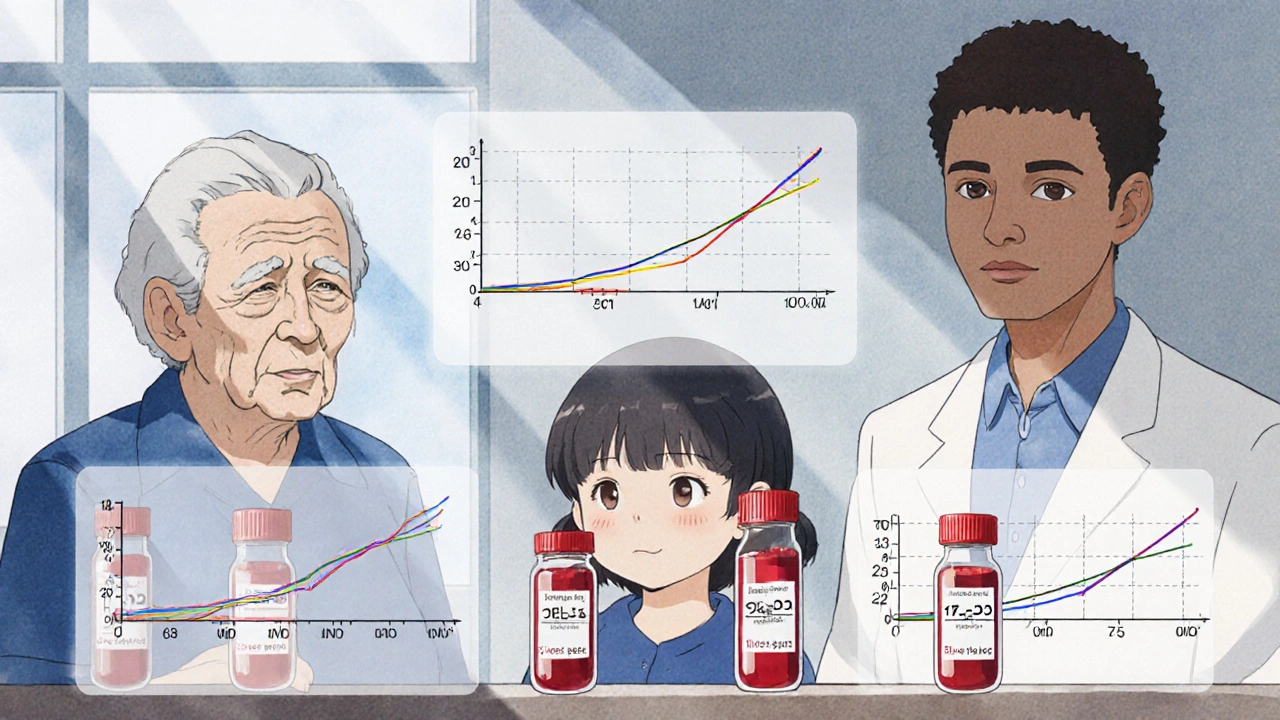
Traditional bioequivalence studies require 24-48 healthy volunteers in a crossover design. Each person gets both drugs, with tight blood sampling schedules. The goal? Show that the average area under the curve (AUC) and peak concentration (Cmax) fall within 80-125% of each other.But here’s the problem: healthy volunteers don’t represent the real world. A drug might be fine in a 25-year-old man, but cause toxicity in an 80-year-old woman with reduced kidney function. Traditional studies miss that.
PopPK doesn’t ignore variability-it measures it. It calculates between-subject variability (BSV), which for many drugs ranges from 10% to 60%. If two formulations have BSV within the same range, and the average exposure is similar, regulators accept that as proof of equivalence. It’s not just about the mean-it’s about the whole distribution.
For drugs with a narrow therapeutic index-like warfarin, digoxin, or certain epilepsy meds-this matters even more. A 10% difference in exposure might mean the difference between a seizure and an overdose. PopPK gives you the tools to see that risk across the population, not just in a few lab subjects.
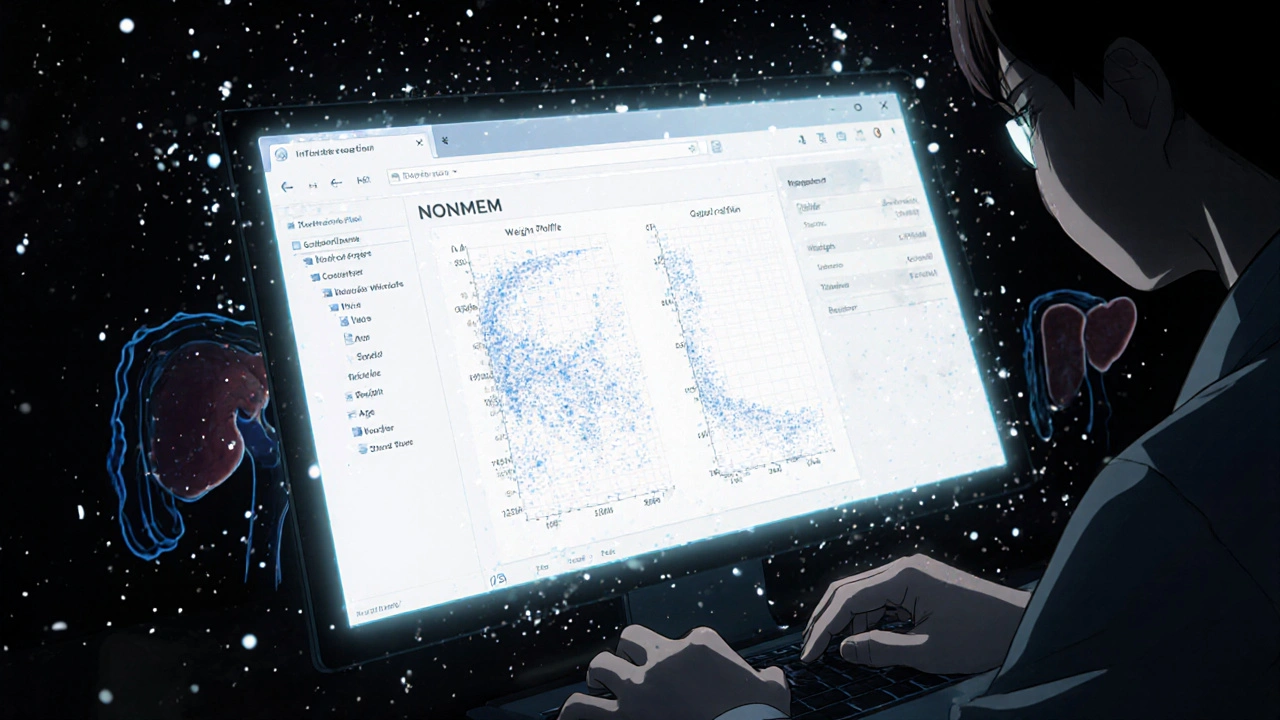
The Tools and Skills Behind PopPK
You can’t run a PopPK analysis with Excel. It requires specialized software: NONMEM (used in 85% of FDA submissions), Monolix, or Phoenix NLME. These programs handle complex math that models how each patient’s drug levels change over time, while accounting for differences in age, weight, organ function, and more.But software alone isn’t enough. You need people who know how to build, validate, and interpret these models. It takes 18 to 24 months of focused training for a pharmacokineticist to become proficient. And even then, mistakes happen.
A 2019-2021 review of FDA rejection letters found that 30% of PopPK submissions needed more information-mostly because of overcomplicated models, poor data quality, or lack of validation. The biggest pitfall? Building a model that fits the data too well but doesn’t reflect reality. That’s called overparameterization. It looks impressive on paper, but fails when tested against new data.
Successful PopPK studies start early. The FDA recommends planning the data collection during Phase 1 clinical trials, not waiting until the end. That means designing studies with PopPK in mind: collecting samples at different times, across different patient groups, and recording all relevant covariates like lab values and concomitant medications.
Where PopPK Falls Short
PopPK isn’t a magic bullet. For drugs with extremely high variability-like some anticoagulants or anti-seizure meds-traditional replicate crossover designs still give more precise estimates of within-subject variability. PopPK struggles when data is too sparse or poorly collected. If you only have one sample per patient, and no info on kidney function or weight, the model can’t do much.Another issue? Validation. There’s still no universal standard for how to prove a PopPK model is reliable. Some use bootstrapping. Others use visual predictive checks. The lack of consensus means regulatory reviewers sometimes disagree on whether a model is acceptable. That’s why companies like Pfizer and Merck have developed their own internal guidelines to ensure consistency.
And while the FDA is open to PopPK-only equivalence claims, some EMA committees still prefer traditional data. A senior pharmacometrician on Reddit shared in 2023 that regional differences in acceptance remain a real hurdle.
Real-World Impact: From Bench to Bedside
One of the most powerful uses of PopPK is in pediatric and geriatric populations. Imagine trying to test a new epilepsy drug in newborns. You can’t take 10 blood samples from a 3-day-old baby. It’s unethical. But if you collect 1-2 samples from 50 infants across multiple hospitals-along with their weight, gestational age, and liver enzyme levels-you can build a PopPK model that predicts the right dose for each baby. That’s exactly how some neonatal drug dosing guidelines were developed.Same with kidney disease. Traditional bioequivalence studies exclude patients with severe renal impairment. PopPK lets you include them. One study showed that a generic version of a blood pressure drug had equivalent exposure in patients with stage 3-4 kidney disease, based on PopPK modeling of real-world data. No additional trials needed.
Even biosimilars-complex biologic drugs that mimic reference products-are increasingly approved using PopPK. Traditional methods don’t work well for large molecules like antibodies. PopPK, combined with clinical outcome data, has become the go-to method for proving they behave the same way in patients.
The Future: AI and Global Harmonization
The next wave is machine learning. A January 2025 paper in Nature showed how AI can detect hidden, non-linear relationships between patient traits and drug clearance-like how a combination of low albumin and high creatinine might uniquely affect a drug’s metabolism. Traditional models might miss that. AI spots it.Also, the IQ Consortium’s Pharmacometrics Leadership Group is working on standardizing model validation by late 2025. That’s a big deal. If everyone agrees on what ‘good enough’ looks like, regulators will accept PopPK claims faster and more consistently.
And the market is growing. The global pharmacometrics market-driven by PopPK-is projected to hit $1.27 billion by 2029. Nearly all top pharmaceutical companies now have dedicated pharmacometrics teams, up from just 65% in 2015. This isn’t a niche tool anymore. It’s central to how drugs are developed and approved.
Final Thoughts: It’s Not About Replacing, But Enhancing
PopPK doesn’t make traditional bioequivalence studies obsolete. But it does make them unnecessary in many cases. For simple, well-behaved drugs in healthy adults, the old method still works fine. But for complex drugs, special populations, or biosimilars, PopPK is the only way to prove true therapeutic equivalence.It turns data from scattered clinic visits into a powerful tool for patient safety. It shifts the focus from ‘average equivalence’ to ‘consistent exposure across diverse people.’ And it’s helping get the right dose to the right patient-faster, cheaper, and more ethically.
If you’re involved in drug development, regulation, or even just prescribing medications, understanding PopPK isn’t optional anymore. It’s how the future of medicine is being built.
What is the main advantage of population pharmacokinetics over traditional bioequivalence studies?
The main advantage is that PopPK uses real-world data from diverse patient groups-including elderly, children, and those with organ impairment-where traditional studies can’t ethically or practically be done. Instead of relying on healthy volunteers with dense blood sampling, PopPK analyzes sparse data from routine clinical care to show how drug exposure varies across populations and whether differences between formulations are clinically meaningful.
Can PopPK be used to prove bioequivalence for generic drugs?
Yes. The FDA and EMA now accept PopPK data as part of regulatory submissions for generic drugs, especially when the target population is heterogeneous or the drug has a narrow therapeutic index. In cases where traditional bioequivalence studies are impractical-like for drugs used in kidney failure or neonates-PopPK can replace them entirely, provided the model is well-validated and supported by sufficient data.
What software is used for population pharmacokinetic modeling?
The most widely used software includes NONMEM (used in 85% of FDA submissions), Monolix, and Phoenix NLME. These tools handle nonlinear mixed-effects modeling, which is essential for analyzing sparse, unbalanced data from real patients. NONMEM remains the industry standard for regulatory submissions due to its long history and validation in regulatory contexts.
How many patients are needed for a reliable PopPK analysis?
The FDA recommends at least 40 participants for robust parameter estimation, but the ideal number depends on the expected variability and the strength of covariate effects. For example, if you’re studying a drug where weight strongly affects clearance, you may need more patients with a wide range of weights. More data isn’t always better-it’s about having the right kind of data collected at the right times.
Why is model validation a challenge in PopPK?
There’s no universal standard for validating a PopPK model. Some use bootstrapping, others use visual predictive checks or simulation-based methods. This lack of consensus leads to inconsistent regulatory reviews. A model that passes in one region may be rejected elsewhere. The IQ Consortium is working to establish standardized validation approaches by late 2025 to reduce this variability.
Is PopPK used for biosimilars?
Yes, PopPK is now a cornerstone of biosimilar approval. Because biologics are large, complex molecules, traditional bioequivalence studies using pharmacokinetic endpoints are often insufficient. PopPK, combined with clinical outcome data, provides the best available method to demonstrate that a biosimilar produces the same exposure profile as the reference product across diverse patient populations.

Kaleigh Scroger
November 28, 2025 AT 14:23PopPK is the future and anyone still clinging to healthy volunteer studies is living in the 90s. I've seen it firsthand in oncology trials where we had 120 patients with wildly different kidney and liver function, and we only needed two sparse samples per person. The model predicted exposure ranges across age, weight, and comorbidities better than any traditional crossover ever could. It's not just convenient-it's ethical. You don't force a 78-year-old with CHF to sit in a clinic for 48 hours getting poked every 30 minutes just to prove a generic works. That's not science, that's torture wrapped in protocol.
Elizabeth Choi
November 30, 2025 AT 09:07Most PopPK models are overfitted garbage. The FDA rejects 30% of submissions for a reason. You throw 20 covariates into NONMEM, call it a 'complex model,' and suddenly you think you've cracked the code. But when you validate it on new data? It collapses. Real-world data is messy. Most companies don't collect the right covariates-no one records adherence, diet, or even time of day the sample was taken. PopPK doesn't fix bad data, it just hides it with math.
Allison Turner
December 1, 2025 AT 01:13So you're telling me we can skip real trials now? Just run some math on half-assed clinic samples and say 'yep, same drug'? Sounds like a shortcut for Big Pharma to save money while patients get screwed. I've seen generics cause seizures because the model didn't account for how people actually take their meds-like skipping doses or crushing pills. PopPK looks fancy but it's just corporate smoke and mirrors.
Darrel Smith
December 1, 2025 AT 16:31This is how they control us. First they take away our right to know what's in our meds. Then they say 'trust the algorithm.' Now they're using math to hide the fact that generics aren't the same. They don't test on real people with real problems-they test on a spreadsheet. And if your kidney function drops 10%? The model says 'still fine.' But your body says 'I'm dying.' This isn't progress. It's surrender to corporate greed wrapped in a white coat.
Aishwarya Sivaraj
December 2, 2025 AT 04:25PopPK is beautiful really. It lets us see the human behind the data. I worked on a project in Mumbai where we collected samples from diabetics with kidney issues who came to the clinic once a month. No one had ever modeled their drug levels before. The model showed that even small changes in protein intake affected clearance. That changed how we dosed them. It's not just about equivalence-it's about dignity. We stopped treating them as outliers and started seeing them as individuals with patterns. The math just helped us listen better
Iives Perl
December 2, 2025 AT 15:31NONMEM is a CIA tool. They use it to track your meds and predict when you'll overdose. You think this is science? It's surveillance. They collect your samples, your weight, your lab values, your meds, your coffee habits-everything. And then they sell it to insurers. PopPK isn't helping patients. It's building a database to deny care. I've seen the contracts. They're not in the public record. But I have screenshots. 🕵️♂️
steve stofelano, jr.
December 2, 2025 AT 22:46It is with considerable respect for the evolving standards of regulatory science that I acknowledge the paradigm shift represented by population pharmacokinetic modeling. The integration of sparse sampling, covariate analysis, and nonlinear mixed-effects methodology constitutes a significant advancement in therapeutic equivalence assessment. This approach not only enhances the precision of dose individualization but also aligns with the principles of patient-centered care and ethical research conduct. The global harmonization of validation criteria, as proposed by the IQ Consortium, is a most commendable initiative that shall undoubtedly elevate the integrity of pharmacometric science.
Savakrit Singh
December 3, 2025 AT 23:54PopPK is the future, but only if you have clean data. In India, we get one sample per patient, no weight, no labs, no meds list. The model just guesses. It's like using a broken thermometer to decide if someone has a fever. Still, regulators love it because it looks fancy. 📈📊
Cecily Bogsprocket
December 4, 2025 AT 20:16I think what's beautiful about PopPK is that it forces us to ask: who are we really serving? The healthy 25-year-old man in the lab? Or the 82-year-old woman with three chronic conditions taking eight pills a day? The old way ignored her. PopPK doesn't just include her-it listens to her. It sees that her body isn't broken, it's different. And that difference isn't noise-it's data. That's not just science. That's compassion with algorithms.