Drug Equivalence: What Makes Medications Interchangeable and Safe
When you pick up a prescription, you might see a different name on the bottle than what your doctor wrote. That’s often because of drug equivalence, the scientific standard that ensures one medication performs the same way in the body as another, even if it’s made by a different company. Also known as bioequivalence, it’s the invisible rule that lets pharmacies swap brand-name pills for cheaper generics without risking your health. But not all swaps are created equal. Some generics work fine. Others don’t. And knowing the difference can save you from side effects, wasted money, or even hospital visits.
Drug equivalence isn’t just about having the same active ingredient. It’s about how fast your body absorbs it, how much of it actually gets into your bloodstream, and whether it behaves the same way over time. The FDA requires generics to match brand drugs within a narrow range—usually 80% to 125% of the original’s effect. That sounds strict, but for some drugs, even small differences matter. Think blood thinners, seizure meds, thyroid pills, or antidepressants. A 10% drop in absorption might mean your condition flares up. A 15% spike could cause dizziness or worse. That’s why bioequivalence, the measurable proof that two drugs deliver the same therapeutic result isn’t just paperwork—it’s your safety net.
Then there’s the gray zone: authorized generics, brand-name drugs made by the same company but sold under a generic label, often at a higher price than true generics. They’re chemically identical to the brand, but you’re paying more because the company owns both. Meanwhile, true generics from independent makers can vary slightly in fillers, coatings, or release rates. These don’t change the active drug—but they can change how it feels to take it. Some people report different side effects, even when the FDA says the drugs are equivalent. That’s why keeping a personal medication list, a real-time record of every pill, supplement, and OTC drug you take helps you spot changes early.
And here’s the thing: drug equivalence doesn’t guarantee you’ll feel the same. Your body might respond differently to a generic version just because of how your stomach processes it. That’s why pharmacists are your best ally. They track which brands and generics work for you, and they’ll warn you if a switch could cause trouble. A 2023 study found that patients who asked their pharmacist about generic switches had 30% fewer unexpected side effects than those who didn’t. It’s not magic—it’s just knowing who to ask.
Below, you’ll find real-world guides on how to spot unsafe swaps, understand why some generics cost more than others, and when to push back if a new pill feels off. You’ll learn how patent battles affect what’s on your shelf, how to read drug labels like a pro, and why some medications simply shouldn’t be swapped at all. Whether you’re on a tight budget or just want to make sure your treatment stays effective, this collection gives you the tools to ask the right questions—and get the right answers.
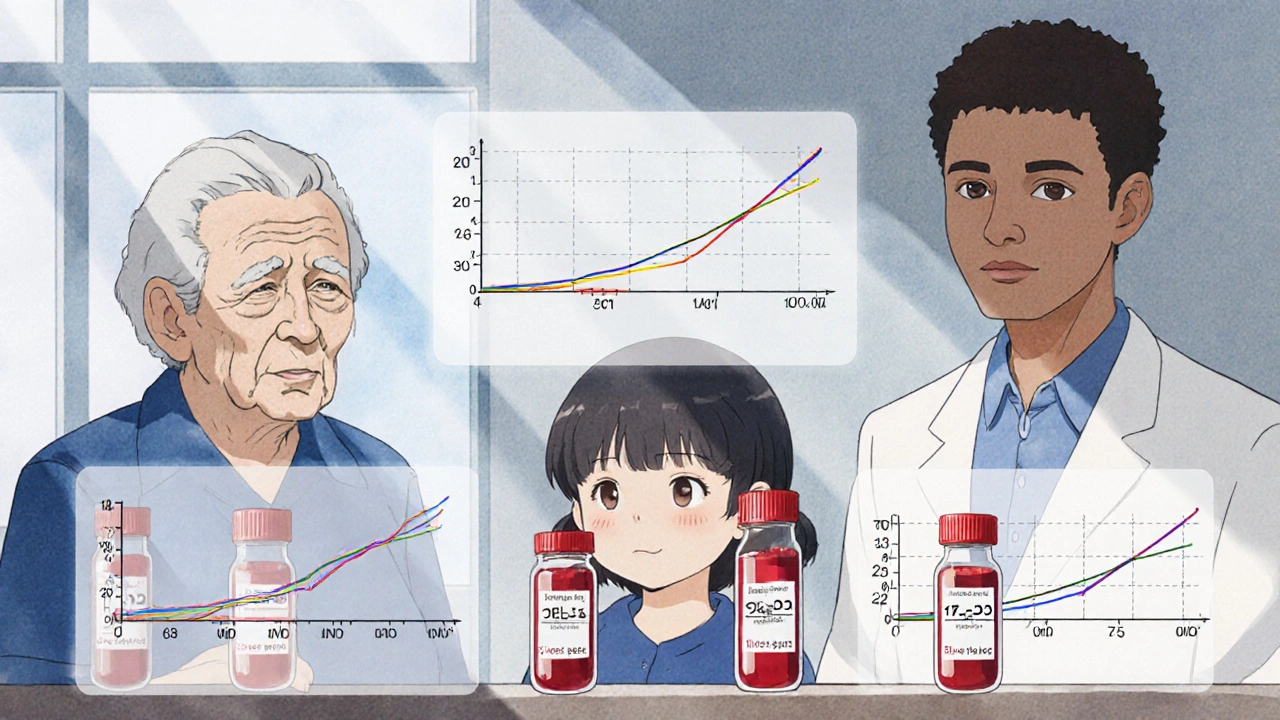
Population Pharmacokinetics: How Data Proves Drug Equivalence Beyond Traditional Bioequivalence Studies
Population pharmacokinetics uses real-world patient data to prove drug equivalence across diverse populations, offering a more accurate and ethical alternative to traditional bioequivalence studies.
