Kidney Stone Treatment Estimator
Stone Size Assessment
Enter the diameter of your kidney stone in millimeters to get personalized treatment recommendations.
Treatment Recommendations
Enter your stone size to see treatment options.
Prevention Tips
Maintain these habits to reduce recurrence risk:
- Drink 2.5-3L water daily
- Limit sodium to < 2g per day
- Balance calcium intake from food
Imagine a sudden, stabbing pain in your back that radiates to the groin, accompanied by nausea and an urgent need to pee. That’s often the first signal that a kidney stone is trying to make its way out. Catching it early can mean the difference between a quick, minimally invasive fix and weeks of agony, costly procedures, and time off work. This guide walks you through why spotting stones early matters, how doctors diagnose them, and which treatments get you back to normal fast.
What Are Kidney Stones?
Kidney stones are hard mineral deposits that form inside the kidneys when urine becomes supersaturated with certain salts. They range from tiny “grains of sand” to larger than a pea, and the most common composition is calcium oxalate, followed by uric acid, struvite, and cystine. When a stone blocks the urinary tract, the pressure builds, triggering the intense pain known as renal colic.
How Early Detection Saves You Pain and Money
Most people assume that waiting until the pain peaks is the only way to know a stone is present. In reality, early detection can cut treatment costs by up to 40% and reduce hospital stays dramatically. When a stone is caught while still small (usually under 5 mm), doctors can often dissolve it with medication or crush it non‑invasively, avoiding surgery altogether. Early spotting also prevents complications like infection, kidney damage, or the formation of multiple stones.
Warning Signs You Shouldn’t Ignore
- Sharp flank pain that may move toward the lower abdomen or groin.
- Blood in the urine (pink or cola‑colored urine).
- Frequent urge to urinate with only a small amount passed.
- Nausea, vomiting, or sweating without an obvious cause.
- Fever or chills - could signal a concurrent infection.
If any of these symptoms surface, especially after a period of low fluid intake, it’s time to get checked.
Diagnostic Tools: Spotting Stones Early
Doctors have several imaging options, each with its own strengths. The table below breaks down the most common methods.
| Method | Radiation | Sensitivity (detects >3 mm) | Cost (AUD) | Typical Availability |
|---|---|---|---|---|
| CT scan - non‑contrast helical computed tomography | High | 98 % | 250-350 | Hospital radiology departments |
| Ultrasound imaging - renal and pelvic ultrasound | None | 70‑85 % | 120-180 | Clinics, emergency rooms |
| X‑ray (KUB) | Moderate | 50‑60 % | 80-120 | Most medical centers |
| Intravenous pyelogram (IVP) | Moderate | 70 % | 200-300 | Specialized radiology units |
For most adults, a low‑dose CT scan is the gold standard because it spots even tiny stones and provides 3‑D mapping for treatment planning. However, ultrasound is a great radiation‑free alternative for pregnant patients or children.
Treatment Options: From Shock Waves to Surgery
Once a stone is identified, the treatment path depends on size, location, and composition. Below is a quick side‑by‑side look at the main approaches.
| Treatment | Best For Stone Size | Invasiveness | Typical Recovery | Success Rate |
|---|---|---|---|---|
| Extracorporeal shock wave lithotripsy - uses focused sound waves to break stones into passable fragments | 4‑10 mm | Non‑invasive | 1‑2 days | 85‑90 % |
| Ureteroscopy - thin scope passed through urethra to retrieve or laser‑break stones | 5‑20 mm ( ureter ) | Minimally invasive | 2‑4 days | 90‑95 % |
| Percutaneous nephrolithotomy (PCNL) | >20 mm | Invasive (small incision) | 5‑7 days | 95‑98 % |
| Medical expulsive therapy (MET) | ≤5 mm | Oral medication only | Varies (days‑weeks) | 70‑80 % (if stone passes) |
| Observation & hydration | ≤3 mm | None | Spontaneous passing | 60‑70 % |
Small stones often pass with plenty of water and a short course of pain relievers. Larger or stubborn stones usually need shock‑wave lithotripsy or ureteroscopy. In rare cases where the stone is massive or infected, PCNL becomes the go‑to.
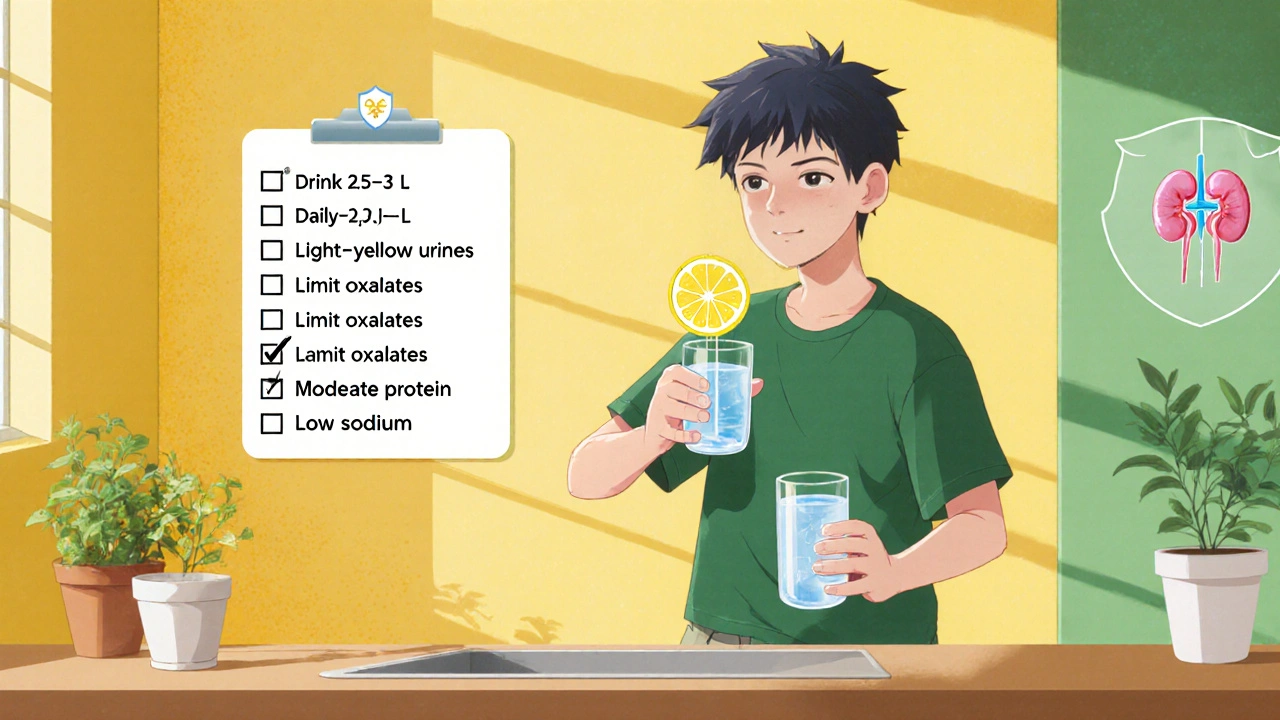
Lifestyle Changes to Prevent Recurrence
Even after successful treatment, the chances of forming another stone stay high-up to 50 % within five years. Making a few daily tweaks can slash that risk dramatically.
- Hydration: Aim for at least 2.5‑3 L of fluid daily; urine should be light yellow.
- Calcium balance: Don’t cut calcium outright; consume 1,000‑1,200 mg from foods like dairy or fortified alternatives.
- Limit oxalates: Reduce high‑oxalate foods such as spinach, nuts, and chocolate if you form calcium oxalate stones.
- Control protein: Excess animal protein raises urine calcium and uric acid. Keep meat portions moderate.
- Watch sodium: High salt boosts calcium excretion; stay under 2 g of sodium per day.
- Monitor medication side‑effects: Certain diuretics and antacids can raise stone risk; discuss alternatives with your doctor.
For patients with Calcium oxalate stones - the most prevalent type, formed from calcium combined with oxalate, diet tweaks are especially critical. Those prone to Uric acid stones - often linked to high purine intake and low urine pH benefit from alkalinizing their urine with potassium citrate.
Quick Checklist: Early Detection and Action Steps
- Notice any flank pain, blood in urine, or sudden urgency? Schedule a doctor visit.
- Ask for a low‑dose CT scan if you’re an adult; opt for ultrasound if pregnant.
- If stone is ≤5 mm, discuss MET or increased water intake before jumping to procedures.
- For stones >5 mm, ask about shock‑wave lithotripsy or ureteroscopy.
- After treatment, keep a fluid diary for two weeks to confirm you’re drinking enough.
- Schedule a follow‑up imaging test in 4‑6 weeks to ensure no residual fragments.
Frequently Asked Questions
Can kidney stones be detected without imaging?
Early symptoms like severe flank pain, hematuria, and frequent urination can raise suspicion, but imaging (CT or ultrasound) is needed for a definitive diagnosis.
How long does shock‑wave lithotripsy take?
The procedure itself lasts about 15‑20 minutes. You’ll usually go home the same day and may need a few days of pain relief.
Are there home remedies that actually work?
Drinking plenty of water and taking over‑the‑counter pain relievers can help symptoms, but they won’t dissolve a stone. Lemon juice (citric acid) may help prevent calcium‑based stones, but consult a doctor before trying any regimen.
When is surgery unavoidable?
If a stone is larger than 2 cm, causes persistent infection, or blocks urine flow despite other treatments, surgical options like PCNL become necessary.
What follow‑up care is needed after stone removal?
Patients should drink ample fluids, repeat imaging after 4‑6 weeks, and discuss dietary adjustments based on stone composition to lower recurrence risk.

Monika Bozkurt
October 19, 2025 AT 15:53Early identification of nephrolithiasis enables clinicians to stratify patients based on stone size, composition, and anatomical considerations, thereby optimizing therapeutic algorithms. By leveraging low‑dose computed tomography, practitioners can obtain high‑resolution volumetric data while mitigating radiation exposure relative to conventional protocols. Moreover, the integration of metabolic panels facilitates targeted prophylaxis, reducing recurrence rates in susceptible cohorts. The overarching paradigm underscores a shift from reactive intervention to proactive management, aligning with evidence‑based guidelines. Ultimately, such a systematic approach enhances patient outcomes and curtails healthcare expenditures.
Catherine Viola
October 22, 2025 AT 04:26While the clinical merit of low‑dose CT is undeniable, one must remain vigilant regarding the insidious proliferation of ionizing radiation in contemporary diagnostics. Industry lobbyists have historically downplayed cumulative dose implications, fostering a culture of complacency among providers. Independent epidemiological data suggest a non‑trivial correlation between repeated imaging and long‑term oncogenic risk, particularly in younger demographics. Consequently, a judicious appraisal of imaging necessity should be embedded within each patient encounter, prioritizing ultrasound when clinically feasible. Such prudence safeguards both individual health and systemic integrity.
sravya rudraraju
October 24, 2025 AT 13:23From a holistic standpoint, the imperative of early nephrolithiasis detection extends beyond mere symptom mitigation; it fundamentally reshapes the therapeutic trajectory by harnessing minimally invasive modalities before irreversible renal compromise ensues. When a stone is identified while measuring less than five millimeters, the therapeutic armamentarium includes medical expulsive therapy, wherein alpha‑blockers facilitate ureteral smooth muscle relaxation, thereby expediting natural passage. Conversely, stones marginally larger, occupying the 5‑10 millimeter window, become amenable to extracorporeal shock wave lithotripsy, a non‑invasive technique that harnesses focused acoustic energy to fragment calculi into passable shards, drastically reducing hospital stay durations. Should these approaches prove insufficient, ureteroscopy offers a conduit for direct laser lithotripsy, granting precise fragmentation and retrieval, albeit with a modestly increased invasiveness profile. It is paramount to recognize that each intervention carries distinct risk‑benefit matrices, necessitating individualized decision‑making predicated upon stone composition, anatomical location, and patient comorbidities. Beyond the acute management, long‑term prophylaxis hinges upon meticulous dietary modulation; adequate hydration, targeting a urine output exceeding two liters per day, remains the cornerstone of recurrence prevention. Calcium intake, contrary to popular misconception, should not be indiscriminately curtailed; instead, dietary calcium binds intestinal oxalate, attenuating its absorption and subsequent urinary excretion. Simultaneously, patients predisposed to calcium oxalate stones must be counseled to curtail high‑oxalate foods such as spinach, nuts, and chocolate, while also moderating animal protein consumption to avoid hyperuricosuria. Sodium restriction to sub‑2000 milligram daily levels further diminishes urinary calcium excretion, synergistically lowering stone formation propensity. For those with a history of uric acid stones, alkaline urine via potassium citrate supplementation can shift the urinary pH toward a less favorable environment for uric acid precipitation. Periodic metabolic evaluation, encompassing 24‑hour urine collections, facilitates the identification of supersaturation patterns, thereby informing targeted pharmacologic interventions, such as thiazide diuretics for hypercalciuria or allopurinol for hyperuricemia. In aggregate, this multifaceted strategy-encompassing prompt detection, tailored minimally invasive treatment, and rigorous lifestyle adaptation-optimizes patient quality of life while curbing the socioeconomic burden imposed by recurrent nephrolithiasis.
Ben Bathgate
October 26, 2025 AT 18:33Honestly, people jump on CT scans like they're the magic bullet, forgetting there are cheaper, safer ways to spot stones early. Ultrasound can do the job for many, especially if you’re pregnant or just want to avoid extra radiation. Plus, tossing a stone‑breaker at every small rock is overkill when plenty of them just pass with water and a bit of pain meds.
Ankitpgujjar Poswal
October 29, 2025 AT 03:30Enough of the tech‑obsessed hype! If you’re dealing with a sub‑5 mm stone, the first line of defence should be hydration and aggressive fluid intake, not a pricey scan. Drink at least three liters a day, keep your urine pale, and you’ll flush most of those tiny cal‑ox beads right out. Stop buying into the notion that every stone needs a surgical fix; most will dissolve or pass on their own with the right regimen.
Bobby Marie
October 31, 2025 AT 09:40Hydration is key.
Christian Georg
November 2, 2025 AT 18:36Here’s a quick practical tip: set a reminder on your phone to sip water every hour, and keep a reusable bottle on your desk. Adding a splash of lemon can increase citrate levels, which helps prevent calcium stone formation. Also, consider a low‑dose potassium citrate if you’ve had uric acid stones-just check with your doctor first! 😊
Staying consistent with these habits drastically lowers the odds of a painful episode and keeps your kidneys happy.
Christopher Burczyk
November 5, 2025 AT 00:46While the reminder strategy is beneficial, it is essential to emphasize that supplemental citrate should be administered under professional supervision, as indiscriminate use may lead to metabolic alkalosis. Moreover, patient-specific factors such as baseline renal function and electrolyte balance must be evaluated prior to initiating any pharmacologic prophylaxis.
Nicole Boyle
November 7, 2025 AT 09:43Bottom line: catch stones early, stay hydrated, and tailor treatment to the stone’s size and type. Small stones often just need water and a little patience, while larger ones may require shock‑wave or endoscopic methods. Keeping an eye on diet-less salt, balanced calcium, moderate protein-can keep the cycle from repeating.