When you find an old bottle of pills in the back of your medicine cabinet, you might wonder: is it still safe to take? The date printed on the label isn’t just a suggestion-it’s a legal and scientific boundary set by manufacturers. But what does that date actually tell you about safety, effectiveness, and risk? The truth isn’t as simple as ‘expired = dangerous.’ Some drugs stay strong for years. Others turn risky in weeks.
What the Expiration Date Actually Guarantees
The expiration date on your medication isn’t when the drug suddenly stops working. It’s the last day the manufacturer guarantees it will work as intended if stored properly. This date comes from stability testing-where companies expose pills, capsules, and liquids to heat, humidity, and light to see how long they hold up. The U.S. Food and Drug Administration (FDA) requires this testing since 1979. Most drugs are tested under conditions of 25°C (77°F) and 60% humidity, which mimics a cool, dry room. The expiration date is set when the active ingredient drops below 90% of its labeled strength. That’s the threshold for being considered effective.
That doesn’t mean the drug becomes toxic after that date. It means the manufacturer won’t promise it’ll still treat your condition. For chronic conditions like high blood pressure or cholesterol, a small drop in potency might not matter much. But for emergencies-like anaphylaxis or a seizure-it could mean the difference between life and death.
Most Medications Last Way Longer Than the Label Says
Here’s a surprising fact: a 20-year study by the U.S. military, called the Shelf Life Extension Program (SLEP), tested over 3,000 lots of 122 different drugs. The results? About 88% of them were still effective-sometimes even more than 15 years past their expiration date. Ciprofloxacin, a common antibiotic, kept 97% of its strength after 12 years. Amoxicillin, another antibiotic, stayed at 94% potency even after eight extra years.
These weren’t stored in ideal labs. They were kept in military stockpiles under controlled conditions, but still, it shows that expiration dates are often conservative. The FDA itself acknowledges this. In a 2018 guidance document, they noted that many drugs retain potency far beyond their printed date. The problem? The law requires manufacturers to pick a date they can guarantee. They don’t test for 10, 15, or 20 years-it’s too expensive. So they pick a safe window: usually 12 to 60 months.
When Expired Medications Become Dangerous
Not all drugs are created equal. Some degrade fast-and not just in potency. Their chemical structure can change in ways that make them unsafe.
- Nitroglycerin (used for chest pain): Loses half its strength within 3 to 6 months after opening-even before the expiration date. An expired or old nitroglycerin tablet might not stop a heart attack.
- Insulin: Degrades at 1.5% to 2.5% per month if kept above 8°C. A vial left in a hot car or bathroom can become useless quickly. Using degraded insulin can lead to dangerously high blood sugar.
- Liquid antibiotics (like amoxicillin-clavulanate): Once mixed with water, they’re only good for 14 days. After that, bacteria can grow in the liquid. Taking it could make your infection worse.
- Epinephrine auto-injectors (EpiPens): Lose 15% to 20% potency each year after expiration. During a severe allergic reaction, that missing dose could be fatal.
- Warfarin (a blood thinner): Its effect becomes unpredictable when expired. Too little? Risk of clots. Too much? Risk of internal bleeding.
The Institute for Safe Medication Practices calls these Category 1 risks-medications where expiration isn’t just about effectiveness, it’s about safety. If you’re using any of these, don’t gamble. Replace them.
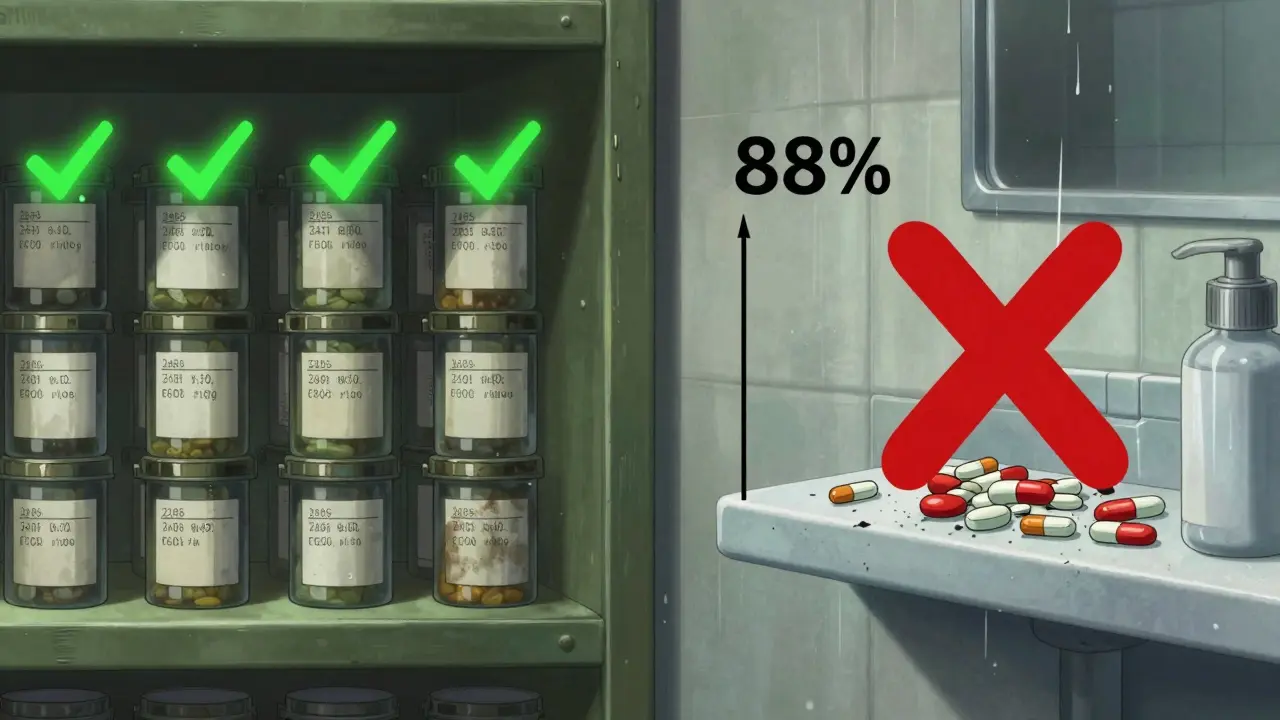
Storage Matters More Than You Think
Your bathroom isn’t the best place to keep medicine. Humidity from showers can reach 75% to 85%. That’s worse than a tropical rainforest for pills. Heat from radiators or sunlight through windows also speeds up degradation.
Studies from the European Medicines Agency show that storing drugs at 30°C instead of 25°C can make them degrade 40% to 60% faster. That means a pill with a 2027 expiration date might lose potency by 2025 if left on a windowsill.
Best practices?
- Keep medications in their original bottles with child-resistant caps sealed.
- Store them in a cool, dry place-like a bedroom drawer, not the bathroom.
- Avoid places near stoves, dishwashers, or windows.
- Don’t transfer pills to pill organizers unless you’re using them within a few weeks. Long-term storage in plastic containers can expose them to moisture.
What Should You Do With Expired Drugs?
Don’t flush most medications. Only specific high-risk drugs-like fentanyl patches or oxycodone tablets-should go down the toilet. The FDA has a Flush List for these. For everything else, use a drug take-back program.
In 2023, the DEA collected over 900,000 pounds of unused medications during National Prescription Drug Take-Back Days. These events happen twice a year. Many pharmacies and police stations also have permanent drop boxes. If you can’t find one, mix pills with coffee grounds or cat litter, seal them in a bag, and throw them in the trash. This makes them unappealing and hard to misuse.
Pharmacies play a big role here. Over 90% of community pharmacies now use “beyond-use” dates-meaning they set a new expiration date when you pick up a prescription. For solid pills, it’s usually one year. For eye drops, it’s 30 days. For liquid antibiotics, it’s 14 days. These dates are often stricter than the manufacturer’s label because they account for how you’ll store it at home.

Is It Ever Okay to Use an Expired Drug?
It depends. For a headache, a slightly expired ibuprofen? Probably fine. For an antibiotic for a serious infection? Not worth the risk. For insulin, EpiPen, or nitroglycerin? Absolutely not.
Some experts, like Dr. Joel Davis at Johns Hopkins, say that for stable conditions like hypertension, a slightly expired ACE inhibitor might be okay for a few days during a shortage-if it’s been stored properly and shows no signs of damage. But that’s a judgment call for a doctor, not a patient.
The bottom line: if the pill is discolored, smells weird, or crumbles, toss it. If it’s been stored poorly, toss it. If it’s for something life-saving, replace it. If it’s a pain reliever you’ve had for two years past the date? It’s probably still fine. But don’t rely on it for anything critical.
The Bigger Picture: Waste, Cost, and Future Changes
Every year, the U.S. throws away $765 billion worth of medication because of expiration dates. That’s 13% to 15% of total drug spending. The military saves $1.2 billion annually by extending expiration dates on stockpiled drugs. Now, new tech is emerging. Smart packaging with time-temperature sensors can now show real-time degradation. In 2023, the FDA started a pilot program using Bluetooth sensors on insulin to update expiration dates based on actual storage. Early results showed a 22% drop in unnecessary discards.
Researchers at the University of Utah are building AI models that predict how long a drug will last based on where it’s been stored. One model got 89.7% accuracy. If this scales up, we might one day see expiration dates that change based on your home environment-not just a fixed date printed in 2022.
For now, though, the safest rule is simple: when in doubt, replace it. Especially for critical meds. Your body doesn’t have a second chance.
Can expired medications make you sick?
Most expired medications won’t make you sick directly, but they might not work. In rare cases, degraded drugs can form harmful compounds-like with tetracycline antibiotics from the 1960s, which caused kidney damage. Modern drugs don’t usually do this, but the risk isn’t zero. The bigger danger is treatment failure: an antibiotic that doesn’t kill the infection, or an EpiPen that doesn’t stop an allergic reaction.
Do all drugs expire at the same rate?
No. Solid pills like aspirin, statins, or antidepressants are very stable and can last years past expiration. Liquids, eye drops, and insulin degrade much faster. Nitroglycerin tablets lose potency in months. Antibiotics in liquid form are only good for two weeks after mixing. Always check the specific drug-don’t assume all pills behave the same.
Is it safe to take expired allergy medicine?
For most people, yes. Antihistamines like loratadine or cetirizine are stable solids and usually retain potency for years. If they look normal and were stored properly, using them a year or two past the date is unlikely to harm you. But if you’re having a severe reaction, don’t risk it-use a fresh one.
Why do pharmacies put shorter expiration dates on prescriptions?
Because the manufacturer’s date is based on ideal storage. Pharmacies know most people store meds in bathrooms or hot cars. To be safe, they set a shorter “beyond-use” date-usually one year for pills, 30 days for eye drops, and 14 days for liquid antibiotics. This reduces the risk of someone taking a weakened or contaminated drug.
Can I extend the life of my medication by storing it in the fridge?
Only if the label says to. Most pills don’t need refrigeration-humidity in the fridge can actually damage them. But insulin, some eye drops, and liquid antibiotics do need cold storage. Always follow the storage instructions on the label. If it doesn’t say “refrigerate,” keep it at room temperature in a dry place.


Lyle Whyatt
February 9, 2026 AT 08:43Okay, I’ll be real-I’ve got a bottle of ibuprofen from 2019 in my sock drawer. I didn’t even know it was there until I found it while looking for socks that don’t have holes. I took one. Didn’t die. Didn’t feel anything different. But honestly? After reading this, I’m gonna toss it. Not because I’m scared it’ll kill me, but because I don’t wanna be the guy who takes expired meds and then tries to explain to his doctor why his headache turned into a full-blown migraine. The military study blew my mind. 15 years past expiration and still working? That’s wild. I feel like we’ve been lied to by Big Pharma for decades. Or maybe they just didn’t wanna pay for longer tests. Either way, I’m not mad. Just… informed. And now I’m cleaning out my medicine cabinet like it’s a Marie Kondo challenge.
Also, bathroom storage? Yeah, that’s my fault. I’ve been keeping my allergy meds next to the shower. No wonder they taste weird now.
PS: If anyone’s got a spare EpiPen they don’t need, I’ll take it. Just kidding. Or am I?
MANI V
February 10, 2026 AT 06:43People really think they can just gamble with their health like this? You wouldn’t eat expired milk, so why do you think pills are different? This isn’t a game. The FDA doesn’t set these dates because they’re lazy-they’re trying to keep you alive. And yet here we are, people treating life-saving drugs like they’re a coupon from 2018. I’m not judging. I’m just stating facts. If you’re too cheap to replace your insulin or EpiPen, maybe you shouldn’t be living with chronic conditions. It’s not rocket science. It’s biology. And biology doesn’t care about your budget.
Also, storing meds in the bathroom? That’s not negligence. That’s a death sentence waiting to happen. You’re basically turning your medicine cabinet into a petri dish. Stop it. Please.
Susan Kwan
February 10, 2026 AT 11:17Oh wow. So the FDA and Big Pharma are in cahoots to make us buy new meds every year? How convenient. Let me guess-next they’ll tell us our toothpaste expires after 30 days too.
Look. I get it. Some drugs are critical. But let’s not turn this into a fear-mongering pamphlet. I’ve taken expired Advil for 10 years. I’ve taken expired Claritin. I’ve taken expired Tylenol. I haven’t died. I haven’t needed ER visits. I have, however, saved hundreds of dollars. So yeah, maybe I’m the exception. But I’m not the only one. And before you start lecturing me about ‘responsibility,’ remind me why the same system that tells me to toss perfectly good meds also charges me $400 for a new prescription with a $1,000 deductible?
Also, ‘don’t flush meds’? Cool. So where do I take them? The nearest drop box is 45 minutes away. And no, I don’t have time to drive there every time I clean out my cabinet. You want me to be responsible? Make it easier. Don’t lecture me.
Random Guy
February 12, 2026 AT 00:25bro i just took a 4 year old xanax and now i’m floating on a cloud of capitalism’s failures
like i knew it was expired but i was like ‘ehhh it’s just a lil chill pill’ and now i’m watching my cat lick the TV and i’m not even mad
also my bathroom is a sauna and my meds are in there like they’re on vacation
anyone else feel like we’re all just one expired antibiotic away from becoming a zombie apocalypse starter?
ps. if you’re reading this and you still use liquid antibiotics past 14 days… we’re not friends anymore
Ryan Vargas
February 12, 2026 AT 08:23The entire pharmaceutical expiration paradigm is a manufactured illusion. It’s not about safety-it’s about profit maximization under the guise of public health. The military’s SLEP program proves, beyond any reasonable doubt, that the degradation curve of most pharmaceuticals is linear and predictable, not catastrophic. Yet, manufacturers are legally shielded from liability if they don’t test beyond 5 years. Why? Because testing for 15, 20, or 30 years would require capital expenditure that cuts into margins. The FDA, bound by regulatory inertia and industry lobbying, refuses to mandate extended stability studies. This isn’t science. It’s corporate policy masquerading as public policy.
And let’s not ignore the psychological component: we’ve been conditioned to fear expiration dates like they’re nuclear launch codes. But the truth? Most solid oral medications retain 90%+ potency for decades if stored in cool, dry, dark conditions. The real danger isn’t the pill-it’s the systemic refusal to acknowledge that science can outpace regulation. We are living in an age where AI can predict drug degradation with 89.7% accuracy, yet we still rely on a 1979 standard that assumes every home is a climate-controlled lab.
Until we decouple expiration from profit motive, we are not just wasting money-we are perpetuating a lie that costs lives through treatment failure, not toxicity. And yes, I’ve read the tetracycline studies. Modern formulations are not 1960s tetracycline. The risk of toxicity is negligible. The risk of underdosing? That’s the real killer.
Tasha Lake
February 14, 2026 AT 06:43Just FYI-the 90% potency threshold isn’t arbitrary. It’s based on pharmacokinetic modeling and bioequivalence thresholds established in the 1980s. Below 90%, the drug’s AUC (area under the curve) and Cmax (peak concentration) fall outside the 80–125% bioequivalence window set by the FDA for generic drugs. So even if a pill ‘seems’ to work, it might not be hitting the therapeutic window consistently. That’s why hypertension meds are tricky-you might think your BP is controlled, but if your lisinopril is at 82% potency, you’re silently at risk for stroke.
Also, refrigeration doesn’t help most solids. Water vapor condensation in fridges can actually accelerate hydrolysis in certain excipients. Only drugs labeled ‘refrigerate’ should go in there. For everything else? Dry, dark, cool. A closet shelf > bathroom > windowsill.
And yes, I’m a pharmacist. No, I don’t sell expired meds. But I do tell patients when it’s safe to use them. Context matters.
Sam Dickison
February 16, 2026 AT 04:01Y’all are overthinking this. I keep my meds in a drawer. No humidity. No sun. No heat. If it looks fine, smells fine, doesn’t crumble? I use it. I’ve got a 6-year-old metformin bottle that still works. My dad’s 8-year-old atorvastatin? Still fine. We’re not lab rats. We’re people. The system is broken. The cost of meds is insane. And if you’re gonna tell me to throw away a $30 bottle because the date says so… then you’re part of the problem.
Also, ‘don’t flush’? Cool. But if I can’t find a drop box and I’m not gonna keep it in my house for another decade? What’s the alternative? Burn it? Bury it? I’m not gonna risk my kid finding it. So I flush the ones that are on the list. The rest? I toss them in the trash with coffee grounds. Done.
Simple. Practical. Real.
Brett Pouser
February 18, 2026 AT 00:02I’m from a country where meds are expensive and hard to get. We reuse everything. Antibiotics? Reused. Insulin? Reused. Even EpiPens, if they’re not visibly damaged. I know it’s risky. But when you don’t have a choice, you do what you gotta do. I’ve seen people get sick because they couldn’t afford a refill. I’ve seen people die because they waited too long to replace a pill. So yeah, I get why the rules exist. But I also know that in the real world, rules don’t always match reality.
Maybe the answer isn’t ‘always replace.’ Maybe it’s ‘know your meds, know your storage, know your risk.’ And if you’re lucky enough to live somewhere with take-back programs and affordable meds? Then you’re ahead of the game. Don’t forget that.
Karianne Jackson
February 19, 2026 AT 16:06I just threw out my whole medicine cabinet. Like, everything. I was like ‘yikes’ and went full Marie Kondo. Now I’m just sitting here with a pile of pills and a new Amazon order for everything. I’m not even mad. Just… tired. Why does my body need so much stuff? And why does everything expire? I just wanted to be healthy. Not a pharmacist.
Andy Cortez
February 21, 2026 AT 03:12Expire dates are a scam. I’ve been saying this for years. The FDA? Big Pharma? They’re in bed together. They don’t want you to know meds last 15+ years because then you’d stop buying. The military study? Hidden. The AI models? Suppressed. And don’t even get me started on why pharmacies put 1-year dates on prescriptions. It’s not for safety-it’s for profit. You think they care about your health? They care about your credit card. Next thing you know, they’ll say your aspirin expires in 6 months. I’m not taking another pill until we expose this. Someone needs to leak the internal documents. I’m not paranoid. I’m informed.
Jacob den Hollander
February 23, 2026 AT 01:42Hey, I just wanted to say-thank you for writing this. I’ve been a nurse for 18 years, and I’ve seen too many people panic over expired meds… or ignore them completely. This post? It’s balanced. Real. Helpful.
One thing I’d add: if you’re unsure, call your pharmacist. They’re not just there to fill scripts-they’re trained to answer questions like this. No judgment. No shame. Just facts.
And if you’re storing meds in the bathroom… I get it. It’s convenient. But try a drawer. It’s not a huge change. But it could save your life-or someone else’s.
Also, if you’re ever in doubt? Replace it. Especially for insulin, EpiPens, or heart meds. It’s not expensive compared to an ER visit. And you deserve to feel safe.
You’re not alone in this. We’re all just trying to take care of ourselves. And you’re doing better than you think.