Evidence-Based Supplements: What Works, What Doesn’t, and How to Choose
When you hear evidence-based supplements, dietary products supported by peer-reviewed clinical studies rather than marketing claims. Also known as science-backed supplements, they’re the difference between spending money on hope and investing in real results. Too many products claim to boost energy, shrink belly fat, or cure joint pain—but only a small fraction have been tested in humans under controlled conditions. The rest? They’re built on anecdotes, celebrity endorsements, and vague promises. If you’re trying to make smarter choices for your health, you need to know which supplements actually work—and which ones are just noise.
Take vitamin D, a nutrient critical for immune function and bone health, with strong clinical data supporting its use in deficient individuals. Studies show it reduces respiratory infections in people with low levels, but gives no benefit if you’re already getting enough sun or food. Then there’s omega-3 fatty acids, fish oil compounds linked to lower triglycerides and reduced inflammation in cardiovascular patients. The American Heart Association recommends them for certain heart conditions—not because they’re trendy, but because trials show real outcomes. On the flip side, supplements like colostrum, detox teas, or ‘miracle’ weight-loss pills rarely pass even basic scientific scrutiny. They might be safe, but they’re not effective.
What makes a supplement evidence-based? Three things: peer-reviewed studies, consistent results across multiple trials, and clear dosage guidelines. For example, melatonin, a hormone that regulates sleep, shown in multiple studies to reduce sleep onset time in people with jet lag or insomnia, has well-documented dosing: 0.5 to 5 mg taken 30–60 minutes before bed. Compare that to turmeric capsules with no standardized curcumin content—those are a gamble. The same goes for magnesium, a mineral proven to help with muscle cramps and migraines in people with low levels. But if you’re not deficient, extra magnesium won’t give you more energy—it’ll just give you loose stools.
It’s not just about what you take—it’s about how you take it. Some supplements interact with medications. feverfew, an herb used for headaches, can increase bleeding risk when taken with blood thinners like warfarin. That’s why checking drug interactions matters as much as checking the label. You wouldn’t mix alcohol with Xanax—so why take herbal supplements without knowing their risks? The same caution applies to combining supplements with prescription drugs. DailyMed and FDA databases exist for a reason: to help you avoid dangerous combinations.
What you’ll find in this collection isn’t a list of miracle cures. It’s a practical guide to what science actually supports. From comparing evidence-based supplements like diacerein and glucosamine for arthritis, to understanding how trazodone works with sleep hygiene, or why calcium acetate matters for kidney patients—every post here is grounded in real data, real studies, and real patient outcomes. No fluff. No hype. Just what works, what doesn’t, and how to use it safely.
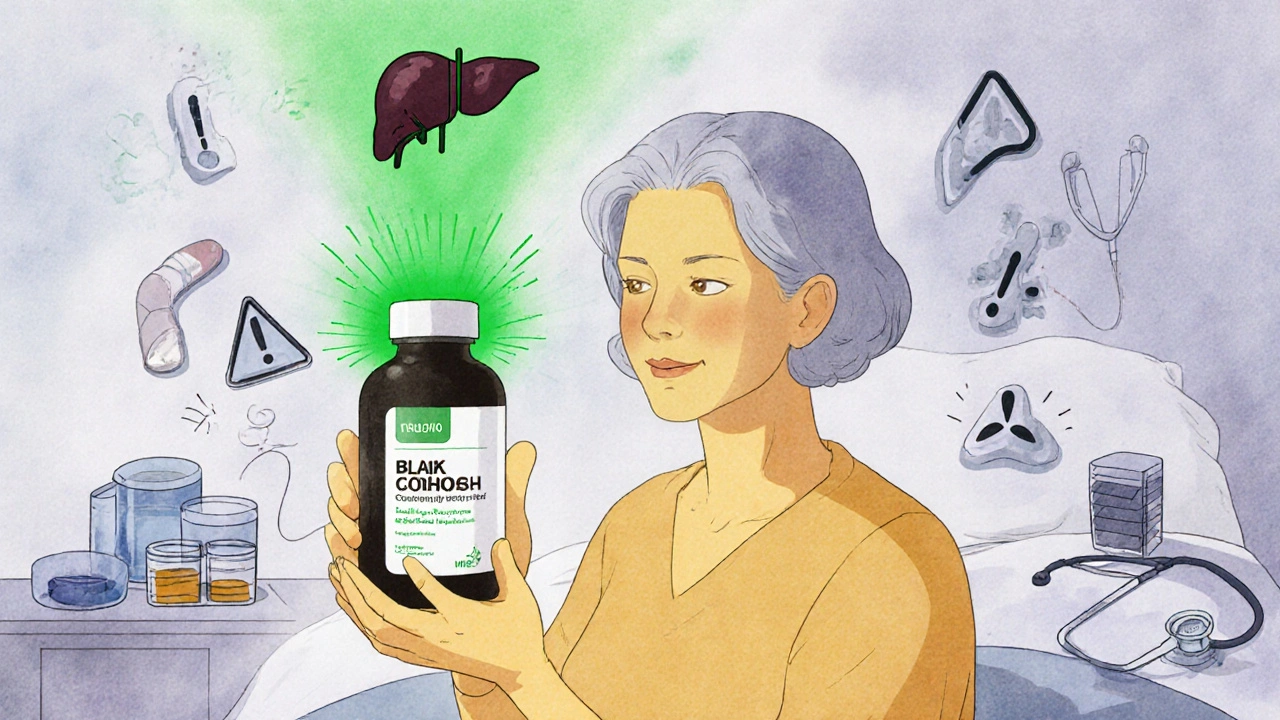
Natural Remedies and Supplements for Side Effects: What’s Backed by Evidence
Natural remedies and supplements aren't always safe - many cause serious side effects or dangerous drug interactions. Learn which ones have real evidence, which ones to avoid, and how to protect yourself.
