Many people turn to St. John’s Wort because they want a natural way to manage mild depression. It’s available over the counter, marketed as safe, and often seen as a gentle alternative to prescription pills. But here’s the truth most labels won’t tell you: St. John’s Wort can dangerously interfere with more than 50 common prescription medications. This isn’t just a theoretical risk. Real people have ended up in hospitals because they didn’t know what they were mixing.
How St. John’s Wort Changes How Your Body Processes Medicines
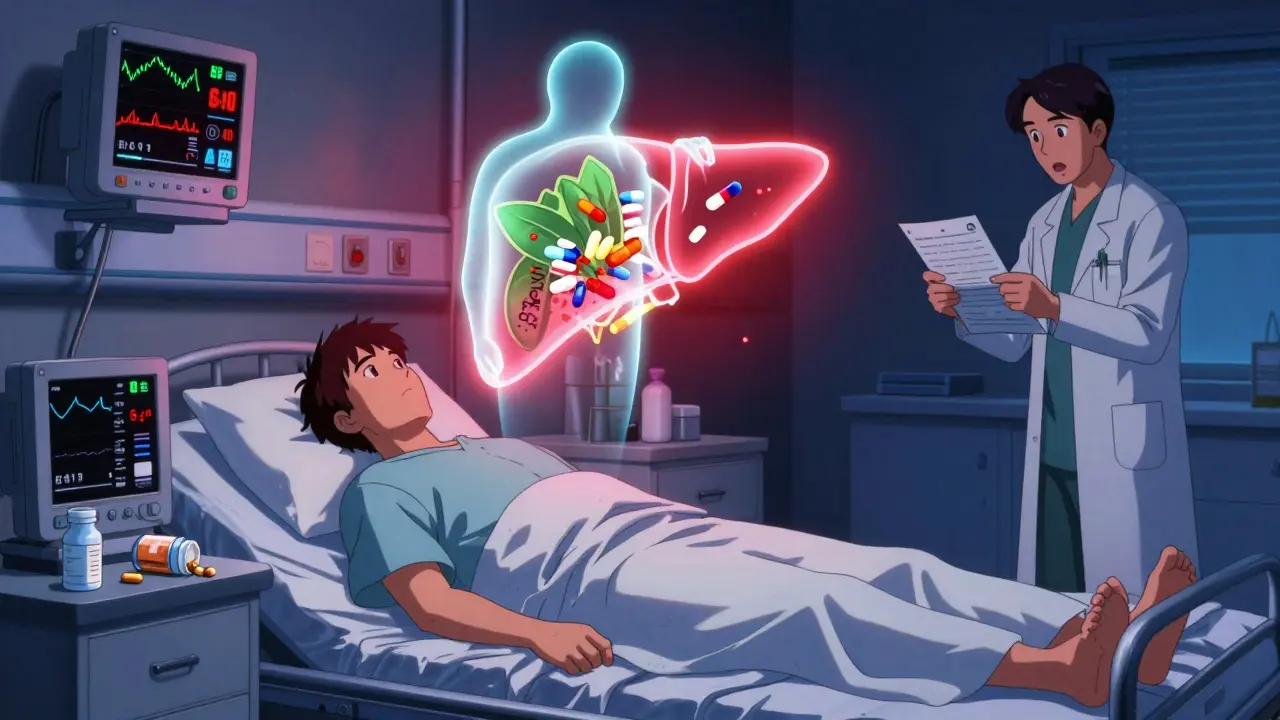
St. John’s Wort doesn’t just sit quietly in your system. It actively tricks your liver into working faster. The active ingredients-mainly hyperforin-turn on enzymes like CYP3A4 and CYP2C9. These are the same enzymes your body uses to break down most drugs. When they’re overworked, your medications get flushed out too quickly.
Think of it like this: if you’re taking warfarin to prevent blood clots, St. John’s Wort can make your body burn through it before it has time to work. That means your blood thickens, and your risk of stroke or clotting goes up. The same thing happens with birth control pills. The hormones get broken down faster, and suddenly, you’re not protected anymore. There are documented cases of unplanned pregnancies in women taking both.
This isn’t a slow, quiet change. The effects can show up in days. And if you stop taking St. John’s Wort? Your body goes back to normal-but the drugs you’re taking don’t. That means their levels can suddenly spike, leading to toxicity. One Australian case report showed cyclosporin levels jumped after someone quit St. John’s Wort, putting a transplant patient at serious risk.
Medications That Can Become Dangerous When Mixed
Here’s a short list of drugs you absolutely shouldn’t mix with St. John’s Wort:
- Antidepressants (SSRIs like sertraline, fluoxetine, or SNRIs like venlafaxine): Combining them can trigger serotonin syndrome-a life-threatening condition with high fever, rapid heart rate, confusion, and muscle rigidity.
- Birth control pills: Even low-dose pills can fail. Breakthrough bleeding and unplanned pregnancies are real outcomes.
- Immunosuppressants (cyclosporin, tacrolimus): Used after organ transplants. If St. John’s Wort lowers their levels, your body may reject the new organ.
- Antiseizure drugs (phenytoin, carbamazepine): These lose effectiveness, leading to breakthrough seizures.
- Anticoagulants (warfarin, rivaroxaban): Increased clotting risk. A single dose change can be deadly.
- HIV medications (protease inhibitors, non-nucleoside reverse transcriptase inhibitors): These can become useless, allowing the virus to rebound.
- Methadone: Used for pain or addiction treatment. St. John’s Wort can make it less effective, leading to withdrawal or increased pain.
- Antipsychotics (clozapine): Levels drop, making symptoms worse.
- Statins (atorvastatin): Reduced cholesterol control.
- Anti-migraine drugs (triptans): Increased risk of serotonin-related side effects.
- Proton pump inhibitors (omeprazole): Reduced effectiveness for acid reflux.
The list goes on. The American Academy of Family Physicians says about half of all prescription drugs are processed by the same liver enzymes St. John’s Wort activates. That means you can’t assume something is safe just because it’s not on a basic list.
Why You Can’t Trust Supplement Labels
Unlike prescription drugs, herbal supplements aren’t held to the same standards. There’s no guarantee that one bottle of St. John’s Wort has the same strength as another. Some contain high levels of hyperforin. Others are weak or even fake. That makes predicting interactions nearly impossible.
Even when labels say “natural” or “safe,” they’re not required to warn you about drug interactions. In countries like Sweden and the UK, manufacturers now include warnings on packaging. In Australia and the U.S., it’s mostly voluntary. You’re left guessing.
And here’s the kicker: many people don’t even tell their doctors they’re taking it. They assume it’s just a “herb,” not a medicine. But if your doctor doesn’t know you’re taking it, they can’t adjust your prescriptions. They can’t monitor your blood levels. They can’t prevent a crisis.
What Happens When You Stop Taking It
Most people think the danger ends when they stop St. John’s Wort. But that’s when the real risk starts.
After you quit, your liver enzymes slowly return to normal. But your other medications? They’re still being taken at the same dose. Now they’re not being broken down as fast. Their levels rise. You could end up with too much of a drug in your system.
One case involved a woman on warfarin who stopped St. John’s Wort and developed dangerous bleeding within days. Another patient on cyclosporin after a kidney transplant saw his drug levels jump 50% after quitting the herb-enough to cause kidney damage.
This is why stopping St. John’s Wort isn’t like stopping a vitamin. It requires medical supervision. Your doctor needs to check your blood levels and adjust your doses over time.
What to Do If You’re Already Taking It
If you’re on St. John’s Wort and any prescription medication, don’t panic-but don’t ignore it either.
- Talk to your doctor or pharmacist. Tell them exactly what you’re taking, including doses and how long you’ve been using it. Don’t say “I take a herbal thing.” Say “I take St. John’s Wort, 300 mg twice a day.”
- Don’t stop suddenly. Abruptly quitting can cause withdrawal symptoms like dizziness, nausea, or irritability.
- Get blood tests. If you’re on warfarin, cyclosporin, tacrolimus, or antiseizure drugs, your levels need to be checked before and after stopping.
- Use a backup birth control method. If you’re on pills, switch to an IUD or condoms until you’ve confirmed it’s safe.
- Monitor for symptoms. Watch for signs of serotonin syndrome: agitation, sweating, fast heartbeat, tremors. Call emergency services if you feel unwell.

Is There a Safe Way to Use St. John’s Wort?
Only if you’re not taking any prescription medications. Even then, it’s not risk-free. Side effects like increased sun sensitivity, dry mouth, dizziness, and anxiety are common. High doses can cause severe photosensitivity-burns from normal sun exposure.
If you have depression, there are safer, better-studied options. Therapy, exercise, and FDA-approved antidepressants have proven results without the hidden dangers. If you’re considering St. John’s Wort, talk to your doctor first. Don’t self-prescribe based on internet reviews or store shelves.
Why This Matters More Than You Think
St. John’s Wort isn’t just another supplement. It’s one of the most dangerous herbal-drug interactions in modern medicine. The Therapeutic Goods Administration in Australia has issued formal alerts. The Mayo Clinic, Merck Manuals, and the AAFP all list it as a high-risk interaction.
Every year, people are hospitalized because they didn’t know. They thought “natural” meant harmless. They didn’t tell their doctor. They didn’t check. And now, they’re paying the price.
The truth? There’s no such thing as a completely safe herbal supplement when you’re on prescription meds. Your body doesn’t care if something is labeled “natural.” It only cares about chemistry. And St. John’s Wort changes the chemistry of your entire medication regimen.
If you’re taking anything prescribed, assume St. John’s Wort is dangerous until proven otherwise. Ask your doctor. Get tested. Don’t gamble with your health.
Can I take St. John’s Wort with antidepressants?
No. Mixing St. John’s Wort with SSRIs or SNRIs can cause serotonin syndrome, a potentially fatal condition. Symptoms include high fever, rapid heart rate, confusion, muscle stiffness, and seizures. Even if you’ve taken both for a while without issues, the risk remains. The American Academy of Family Physicians and the Mayo Clinic both warn against combining them.
Does St. John’s Wort affect birth control?
Yes. St. John’s Wort speeds up the breakdown of estrogen and progestin in birth control pills, patches, and rings. This can lead to breakthrough bleeding or, more seriously, unintended pregnancy. IUDs are not affected because they don’t rely on liver metabolism. If you’re using hormonal birth control and take St. John’s Wort, switch to a non-hormonal method like a copper IUD or condoms until you’ve talked to your doctor.
How long does St. John’s Wort stay in your system?
The active compounds, especially hyperforin, can induce liver enzymes for up to two weeks after you stop taking it. This means drug interactions can continue even after you’ve quit. If you’re planning to stop St. John’s Wort before surgery or starting a new medication, give yourself at least 14 days-preferably longer-and get blood tests if you’re on critical drugs like warfarin or cyclosporin.
Can I take St. John’s Wort if I’m on blood pressure medication?
It’s risky. St. John’s Wort can interfere with some blood pressure drugs, especially those metabolized by CYP3A4. It may lower their effectiveness, leading to uncontrolled hypertension. There’s also a risk of sudden drops in blood pressure if you stop the herb while still taking the medication. Always check with your doctor before combining them.
Is St. John’s Wort safe for older adults?
It’s especially dangerous for older adults. Seniors are more likely to be on multiple medications, including blood thinners, heart drugs, and antidepressants. Their livers process drugs more slowly, making interactions harder to predict. The risk of falls, confusion, or internal bleeding increases. Most geriatric guidelines recommend avoiding St. John’s Wort entirely in patients over 65.
What should I tell my pharmacist?
Tell them every supplement you take-no exceptions. Say: “I take St. John’s Wort for depression.” Don’t say “I take a herbal remedy.” Pharmacists have access to interaction databases and can flag dangerous combinations before you pick up your prescription. Many don’t ask unless you tell them. Don’t wait for them to ask.
Are there safer herbal alternatives for depression?
There’s no herbal supplement proven to be both safe and effective for depression without interaction risks. Omega-3 fatty acids, vitamin D, and exercise have shown mild benefits in studies, but none replace prescribed treatment. If you’re struggling with depression, talk to your doctor about therapy or FDA-approved medications. The risks of unregulated herbs far outweigh the benefits.
Next Steps: Protect Yourself
If you’re taking any prescription drugs, stop using St. John’s Wort until you’ve talked to your doctor. Bring your supplement bottle with you. Write down what you take, how much, and how often. Ask: “Could this interfere with my other meds?”
Don’t rely on internet forums or store clerks. Your health isn’t a guess. It’s a science. And St. John’s Wort? It’s one of the most scientifically proven herbal dangers out there.

Ryan Barr
January 7, 2026 AT 01:18St. John’s Wort is the herbal equivalent of a backdoor in your meds. Natural doesn’t mean safe-it means unregulated, unpredictable, and dangerously underestimated.
Dana Termini
January 8, 2026 AT 19:21I had no idea this herb could mess with my birth control until I ended up pregnant. My OB told me to stop it cold turkey-and then we had to monitor my hormones for weeks. This post saved me from a nightmare.
Wesley Pereira
January 9, 2026 AT 07:12Let’s be real-people treat herbal supplements like they’re yoga pants: comfy, harmless, and totally not a pharmacokinetic wildcard. Hyperforin? CYP3A4 induction? Yeah, your ‘natural remedy’ is basically a liver-activating grenade. And no, your Whole Foods clerk isn’t qualified to advise you on drug interactions. Get your ass to a pharmacist.
Isaac Jules
January 10, 2026 AT 00:52LOL you people think you’re being ‘natural’ but you’re just a walking clinical trial for drug toxicity. I’ve seen three patients in the ER this year because they ‘switched from Zoloft to St. John’s Wort for less side effects.’ Guess what? They got serotonin syndrome. One of them had to be intubated. You’re not healing-you’re gambling with your organs. Stop being an idiot.
Stuart Shield
January 11, 2026 AT 16:08There’s something haunting about how we treat herbs like harmless trinkets while treating pharmaceuticals like sacred relics. We’ll trust a pill with a 20-page insert but dismiss a plant because it’s ‘organic.’ The truth? Your body doesn’t care if it came from a lab or a forest-it only cares about the molecules. And St. John’s Wort? It’s a molecular saboteur. I’m glad someone finally spelled it out without the fluff.
Rachel Wermager
January 12, 2026 AT 09:03Actually, the CYP3A4 induction isn’t even the whole story-St. John’s Wort also upregulates P-glycoprotein transporters, which actively efflux drugs out of cells, including the blood-brain barrier. That’s why SSRIs and antipsychotics lose efficacy even faster than you’d expect from hepatic metabolism alone. And the half-life of hyperforin? Up to 72 hours post-ingestion. So if you think stopping it for 48 hours is safe, you’re dangerously misinformed. This isn’t folklore-it’s pharmacology 101.
Leonard Shit
January 12, 2026 AT 23:46yeah i took it for like 3 months while on lisinopril… didn’t think anything of it. then i got dizzy one day and almost passed out. turns out my bp dropped like a rock. my doc said it was probably the herb messing with the cyp3a4 thing. lesson learned: if it’s not on the label as a drug, it’s probably still a drug. oops.
Gabrielle Panchev
January 14, 2026 AT 13:07Okay, but let’s be fair-why are we demonizing St. John’s Wort when the FDA has approved over 500 drugs with worse interaction profiles? And who decided that ‘natural’ equals ‘dangerous’? That’s a cultural bias, not a scientific one. Also, the fact that this post cites the AAFP and Mayo Clinic as gospel ignores the fact that those institutions are funded by pharmaceutical giants who have a vested interest in keeping herbal alternatives off the market. Maybe the real issue is that we’ve been conditioned to distrust anything that doesn’t come with a patent and a price tag. And yes, I’ve read the original studies-hyperforin’s enzyme induction is dose-dependent and reversible, which means, with proper monitoring, it could be used safely. But no, we’d rather just scare people into compliance.
Katelyn Slack
January 14, 2026 AT 16:47i just told my dr i was taking it and she looked at me like i’d confessed to smuggling illegal squirrels. then she wrote me a script for therapy. guess i’m not doing that anymore.