When you're managing type 2 diabetes, finding a medication that lowers blood sugar without causing weight gain or low blood sugar is a win. That’s why SGLT2 inhibitors became so popular. Drugs like canagliflozin, dapagliflozin, and empagliflozin help the kidneys flush out extra glucose through urine. They also reduce heart failure risk and slow kidney damage-proven benefits from big studies like EMPA-REG and DECLARE-TIMI. But there’s a hidden danger that many patients and even some doctors don’t fully understand: diabetic ketoacidosis, especially the sneaky, hard-to-detect version called euglycemic DKA.
What Is Euglycemic DKA, and Why Is It Dangerous?
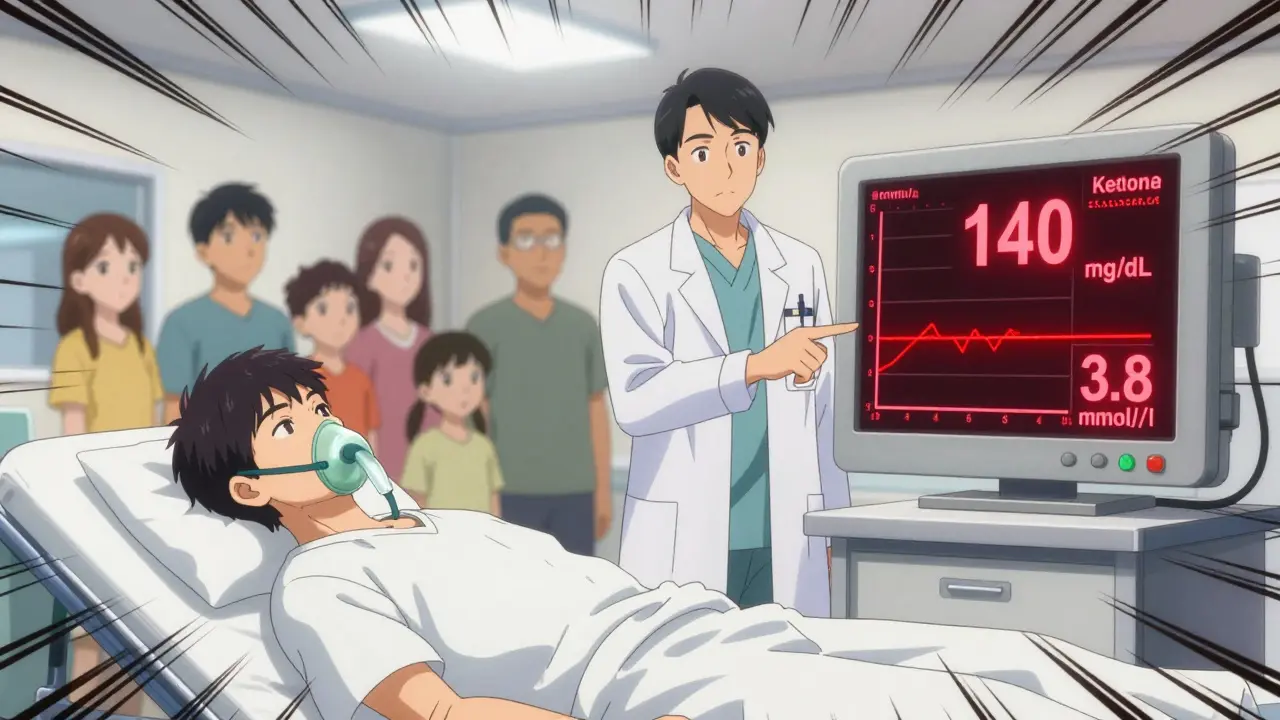
Traditional diabetic ketoacidosis (DKA) looks like this: blood sugar skyrockets above 250 mg/dL, you feel sick, breath smells fruity, and you’re dehydrated. It’s a medical emergency. But with SGLT2 inhibitors, DKA can happen even when your blood sugar is normal-or just slightly high-below 200 mg/dL. This is called euglycemic DKA (euDKA). And it’s dangerous because it slips under the radar.
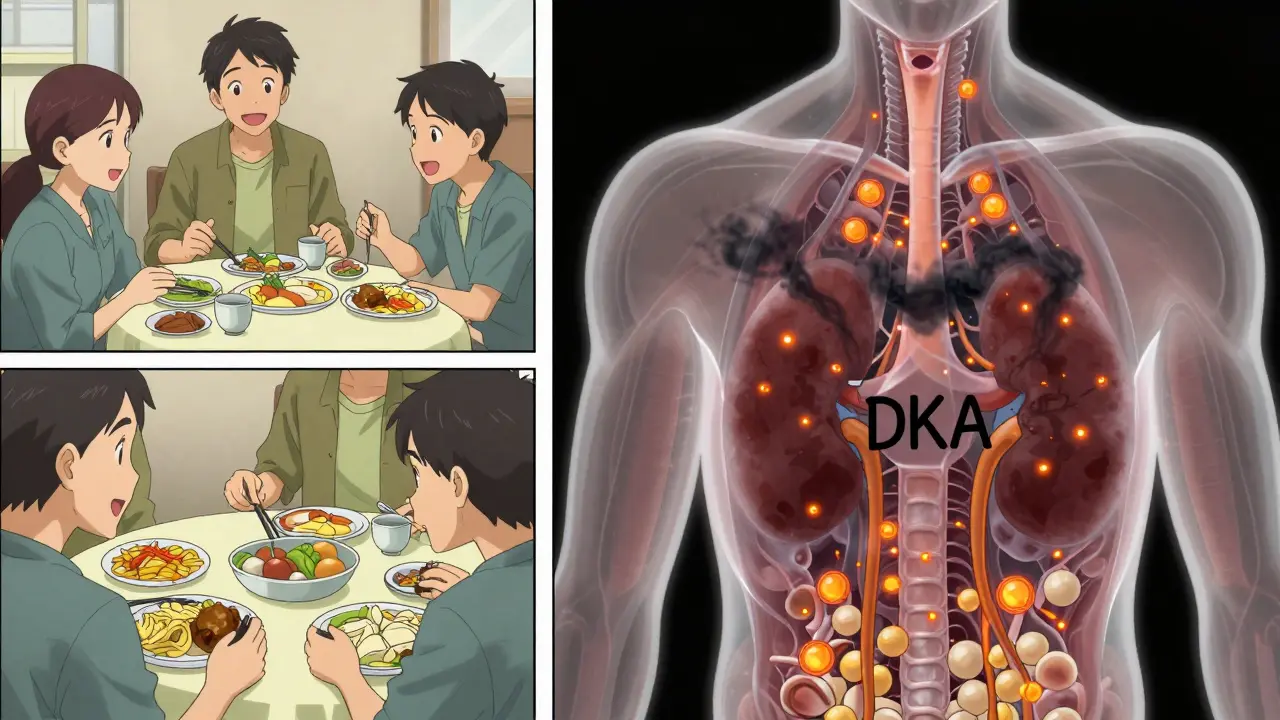
Instead of high glucose, you get ketones building up in your blood. Your body starts burning fat for fuel because insulin isn’t working well enough, even if your sugar levels don’t scream “emergency.” Symptoms? Nausea, vomiting, stomach pain, fatigue, trouble breathing. These can be mistaken for the flu, food poisoning, or just being tired. By the time someone realizes it’s DKA, it’s often advanced.
According to the FDA and European Medicines Agency (EMA), up to 40% of DKA cases linked to SGLT2 inhibitors are euDKA. A 2023 review of over 1,200 reported cases found nearly half had blood sugar under 250 mg/dL. That’s not rare. It’s a pattern.
How Do SGLT2 Inhibitors Cause This?
These drugs work by blocking glucose reabsorption in the kidneys. That sounds good-it lowers blood sugar. But here’s the catch: they also lower insulin levels slightly and increase glucagon, a hormone that tells the liver to make more glucose. When you’re stressed, sick, or not eating enough, your body turns to fat for energy. That’s normal. But with SGLT2 inhibitors, the fat breakdown goes into overdrive, flooding your blood with ketones.
Unlike insulin-dependent type 1 diabetes, where DKA happens fast, SGLT2-related euDKA creeps in. It’s often triggered by something else: an infection, skipping meals, cutting carbs too hard, drinking alcohol, or surgery. One study showed 33% of cases happened during illness, 24% after insulin was reduced, and 15% around surgery.
The risk isn’t the same for everyone. People with low insulin production (low C-peptide levels) are at higher risk. One analysis found that those with C-peptide below 1.0 ng/mL had a 4x higher chance of DKA than those with higher levels. It’s also more common with higher doses-canagliflozin 300 mg carries more risk than 100 mg.
Who’s Most at Risk?
Not everyone on SGLT2 inhibitors will get euDKA. But some groups need to be extra careful:
- People with type 1 diabetes using these drugs off-label (not approved in most countries)
- Those with long-standing type 2 diabetes and declining beta-cell function
- Patients who reduce insulin or carbohydrate intake suddenly
- Anyone preparing for surgery or hospitalization
- People with a history of DKA
- Those who binge on alcohol or have eating disorders
Most cases happen within the first year of starting the drug, with the median time to onset being about 28 weeks. That’s not a fluke-it’s a pattern. And the mortality rate for SGLT2-related DKA is higher than traditional DKA: 4.3% versus 2.1%. Why? Because it’s missed. By the time labs are done, the acidosis is severe.
What Do Doctors Recommend Now?
Guidelines have changed. The American Diabetes Association, the Endocrine Society, and the European Association for the Study of Diabetes all agree: you can’t rely on blood sugar alone to rule out DKA in someone on an SGLT2 inhibitor.
Here’s what they say now:
- Check ketones if you feel nauseous, have abdominal pain, or are unusually tired-even if your glucose is below 250 mg/dL.
- Stop SGLT2 inhibitors at least 3 days before any surgery or procedure requiring fasting.
- Hold the drug during acute illness (like flu, infection, or vomiting).
- Don’t start SGLT2 inhibitors in people with low insulin production or a history of DKA.
A 2022 study in Diabetes Care showed that teaching patients to check ketones at home reduced DKA episodes by 67%. Simple. Effective. Life-saving.
How to Check for Ketones at Home
You don’t need a hospital to spot early warning signs. You can test for ketones at home using:
- Urine strips (like Ketostix)-cheaper, but slower to show changes
- Blood ketone meters (like Precision Xtra)-faster, more accurate, measures beta-hydroxybutyrate
If your ketone level is:
- Trace or small: Drink water, monitor, check again in 2-4 hours
- Moderate or large: Call your doctor or go to the ER-do not wait
Don’t wait for high blood sugar. Don’t assume you’re “just sick.” If you’re on an SGLT2 inhibitor and feel off, test for ketones. It’s the only way to catch euDKA early.
Are These Drugs Still Safe?
Yes-for most people. The benefits are real. SGLT2 inhibitors cut heart failure hospitalizations by 30%, reduce kidney disease progression by 30-40%, and lower cardiovascular death in high-risk patients. The absolute risk of DKA is still low: about 0.1 to 0.5 events per 100 patients per year. That’s rare. But rare doesn’t mean impossible.
Think of it like this: wearing a seatbelt doesn’t guarantee you won’t get hurt in a crash. But it reduces the chance of death. SGLT2 inhibitors are like that. They’re powerful tools, but they need smart use.
Doctors now screen for risk before prescribing. If you have low C-peptide, recent weight loss, or a history of ketoacidosis, they’ll likely choose another class of medication-like GLP-1 agonists or metformin.
What’s Next? New Drugs and Better Tools
Pharmaceutical companies aren’t ignoring this. A new class of drugs called SGLT1/2 dual inhibitors-like licogliflozin-is being tested. Early data suggests they may cause less ketone buildup because they also slow sugar absorption in the gut, which helps stabilize insulin levels.
Machine learning models are also being developed to predict who’s most at risk. A 2024 study in Lancet Digital Health built a tool using 15 factors-age, kidney function, insulin use, BMI, C-peptide levels-and could predict DKA risk with 87% accuracy. That means in the near future, your doctor might run a quick risk score before prescribing.
The FDA and EMA now require all new SGLT2 inhibitor trials to specifically monitor for euDKA. Labels have been updated. Pharmacies now include warning inserts. But the real change has to happen at the patient level.
What You Should Do Right Now
If you’re taking an SGLT2 inhibitor:
- Know the symptoms: nausea, vomiting, stomach pain, fatigue, rapid breathing
- Ask your doctor if you’re at higher risk for euDKA
- Get a ketone testing kit and learn how to use it
- Stop the drug before surgery or during serious illness
- Don’t cut carbs drastically without talking to your care team
- Call your doctor or go to the ER if ketones are moderate or large-even if your blood sugar is normal
If you’re not on one but considering it, ask: “Do I have low insulin production? Have I ever had DKA? Am I willing to check ketones if I get sick?” If the answer is no, there are other options.
SGLT2 inhibitors are not the enemy. But they’re not risk-free. Understanding euDKA isn’t about fear-it’s about control. You’re not just managing blood sugar. You’re managing your whole body’s balance. And sometimes, that means looking beyond glucose.
Can SGLT2 inhibitors cause diabetic ketoacidosis even if my blood sugar is normal?
Yes. This is called euglycemic DKA (euDKA), and it’s a known risk with SGLT2 inhibitors. Blood sugar may be below 250 mg/dL, even as low as 100-150 mg/dL, while ketones rise dangerously. Symptoms like nausea, vomiting, and fatigue can be mistaken for the flu. Always check ketones if you feel unwell, regardless of your glucose level.
How common is DKA with SGLT2 inhibitors?
It’s rare-about 0.1 to 0.5 cases per 100 patients per year. But compared to other diabetes drugs like DPP-4 inhibitors, the risk is nearly 3 times higher. Most cases happen within the first year of use, often triggered by illness, surgery, or reduced food intake.
Should I stop taking my SGLT2 inhibitor if I get sick?
Yes. If you have an infection, vomiting, diarrhea, or are unable to eat normally, stop your SGLT2 inhibitor and contact your doctor. These are major triggers for euDKA. Resume only after you’re back to normal eating and feeling well, and only with your provider’s approval.
Do I need to test for ketones every day?
No. Daily testing isn’t needed unless your doctor advises it. But you should test whenever you feel unwell, have symptoms of DKA, are fasting before surgery, or have reduced your carbohydrate intake. Keep ketone strips or a meter on hand.
Are SGLT2 inhibitors safe for people with type 1 diabetes?
In most countries, SGLT2 inhibitors are not approved for type 1 diabetes. Some doctors prescribe them off-label, but this significantly increases DKA risk. The FDA and EMA warn against their use in type 1 unless under strict supervision with close ketone monitoring and full insulin coverage.
What are the alternatives to SGLT2 inhibitors if I’m worried about DKA?
Metformin remains the first-line choice for most people with type 2 diabetes. GLP-1 receptor agonists like semaglutide or liraglutide offer similar heart and kidney benefits without the DKA risk. DPP-4 inhibitors and insulin are also safe alternatives. Talk to your doctor about your personal risk profile before switching.


Diana Stoyanova
January 8, 2026 AT 10:51Okay but let’s be real-this isn’t just about diabetes meds. It’s about how we’ve been trained to trust numbers over symptoms. I had a friend on dapagliflozin who thought she was just ‘having a bad flu’ for three days. Ketones were through the roof. Blood sugar? 148. She almost didn’t make it. And no one told her to check ketones unless her glucose was above 250. That’s insane. We need to rewire the whole patient education system. It’s not about fear-it’s about empowerment. If you’re on one of these drugs, get a ketone meter. Keep it next to your toothbrush. Test when you feel off. No excuses. Your life isn’t a spreadsheet.
Gregory Clayton
January 10, 2026 AT 00:40Oh great, another ‘pharma conspiracy’ post. Next they’ll say aspirin causes brain rot. SGLT2 inhibitors save lives. People get DKA from skipping insulin, not from the drug. Stop scaring people into thinking every pill is poison. If you’re too weak to handle a little ketone buildup, maybe you shouldn’t be on anything at all. Wake up and stop being a hypochondriac.
Catherine Scutt
January 11, 2026 AT 08:53Gregory, you’re the reason people die. If you think ketones are ‘a little buildup,’ you’ve never seen someone gasping in the ER because their blood pH dropped to 6.9. This isn’t about being ‘weak.’ It’s about biology. And if you’re too lazy to check a simple strip, don’t blame the medicine. Blame yourself for not caring enough to stay alive.
Darren McGuff
January 12, 2026 AT 17:08As a nurse who’s seen over a dozen euDKA cases in the last five years, I can tell you this: the real tragedy isn’t the drug-it’s the lack of follow-up. Patients get prescribed these meds, handed a pamphlet, and told to ‘call if you feel funny.’ That’s not care. That’s negligence. I’ve had patients come in with ketones at 4.8 mmol/L and blood sugar at 130, all because they didn’t know what ‘fatigue’ meant in this context. We need mandatory ketone education at dispensing. Not optional. Mandatory. And pharmacies should be required to hand out a test strip with the first prescription. It costs pennies. Saves lives.
Alicia Hasö
January 13, 2026 AT 16:48Thank you for this comprehensive breakdown. I’ve been a diabetes educator for 18 years, and I can’t tell you how many times I’ve had to explain euDKA to patients who thought ‘normal glucose = safe.’ It’s a silent killer. I now include ketone testing in every new SGLT2 inhibitor prescription plan-whether the patient asks or not. I give them a free strip kit, a laminated symptom card, and a 5-minute video demo. We’ve cut our clinic’s euDKA admissions by 70% since we started. Knowledge isn’t power-it’s protection. And if your doctor isn’t offering this, ask. Politely, but firmly. You deserve to be informed.
Ashley Kronenwetter
January 15, 2026 AT 05:13While the risks are real, the tone of this post is alarmist. The absolute incidence of euDKA remains low, and the cardiovascular and renal benefits are well-documented. Rather than framing SGLT2 inhibitors as dangerous, we should emphasize risk stratification and patient-specific education. Not every patient needs ketone strips-but those with low C-peptide, prior DKA, or planned surgery do. Precision medicine isn’t about fear-it’s about matching interventions to individual biology. Let’s not throw out a powerful tool because a small subset of users need extra caution.
Aron Veldhuizen
January 16, 2026 AT 23:53Let’s deconstruct the logic here. If SGLT2 inhibitors cause euDKA, then why don’t we see the same phenomenon with fasting or ketogenic diets? After all, both induce ketosis. The answer: insulin deficiency. But if the drug lowers insulin slightly, and the body is already insulin-resistant, then why does ketosis occur? The real issue isn’t the drug-it’s the misdiagnosis of insulin resistance as insulin deficiency. We’re conflating physiology with pharmacology. Also, the FDA’s data is self-reported. Many cases are misclassified. And why is there no mention of the fact that DKA incidence has *decreased* overall since these drugs became mainstream? Because mortality from hyperglycemic DKA dropped faster than euDKA rose. This isn’t a crisis. It’s a correction.
Micheal Murdoch
January 17, 2026 AT 22:17Hey everyone-take a breath. This isn’t about being right or wrong. It’s about staying alive. I’ve had patients who were terrified to take their meds after reading scary posts. I’ve had others who ignored warning signs because ‘my sugar’s fine.’ Both are dangerous. Here’s what I tell them: SGLT2 inhibitors are like a sports car. Amazing performance, great fuel efficiency, but if you don’t check the oil, you’re gonna break down. You don’t have to be a mechanic to know when something’s off. If you feel weird-nausea, tired, breathing funny-test your ketones. It takes 10 seconds. No shame. No panic. Just action. And if you’re not sure whether you’re high-risk? Ask your doctor for a C-peptide test. It’s a simple blood draw. It tells you if your body still makes insulin. If it doesn’t, you probably shouldn’t be on this drug. Simple. Smart. Safe. You’re not weak for asking. You’re wise.