When you have an autoimmune disease and are thinking about having a baby, the biggest question isn’t just can I get pregnant? It’s can I stay safe-for me and for my baby-while managing my condition. The old advice used to be: stop everything. But that’s not what the science says anymore. In fact, stopping your meds can be riskier than keeping them.
Why Planning Matters More Than You Think
About 78% of autoimmune diseases are diagnosed in women between 15 and 44. That means most people who live with lupus, rheumatoid arthritis, or psoriatic arthritis are either thinking about pregnancy, planning it, or already pregnant. And yet, nearly half of these women stop their medications on their own-without talking to a doctor-because they’re scared. The truth? Uncontrolled disease is far more dangerous than most medications. A flare during pregnancy can mean preterm birth, preeclampsia, low birth weight, or even miscarriage. One study showed that women with active lupus are three to five times more likely to develop preeclampsia than those whose disease is under control. Hydroxychloroquine, a common lupus drug, cuts that risk in half. This isn’t about being brave. It’s about being smart. The goal isn’t to avoid all meds-it’s to use the right ones, at the right time.What Medications Are Safe? The Clear List
Not all drugs are created equal. Some are safe. Some are not. And some? You need to switch before you even try to conceive. Safe to continue during pregnancy and breastfeeding:- Hydroxychloroquine (Plaquenil): Used for lupus and rheumatoid arthritis. Studied in over 12,000 pregnancies. No increased risk of birth defects. Reduces flares by 66% during pregnancy.
- Azathioprine (Imuran): Common for lupus and inflammatory bowel disease. Safe in over 5,800 pregnancies. Preterm birth risk drops from nearly 9% with active disease to just 2% with this drug.
- Sulfasalazine: Used for rheumatoid arthritis and Crohn’s. Over 3,200 pregnancies show no birth defects.
- Corticosteroids (prednisone, prednisolone): Low doses are fine. Higher doses may raise risks like gestational diabetes, but uncontrolled inflammation is worse.
- TNF inhibitors (adalimumab, etanercept, certolizumab pegol): Collectively studied in over 28,000 pregnancies. Safety rate above 94%. Certolizumab pegol is the safest in the third trimester-it barely crosses the placenta.
What to Avoid-And When to Switch
Some drugs are outright dangerous during pregnancy. If you’re on one of these, you need to switch before you get pregnant.- Methotrexate: A common RA drug. Causes severe birth defects-craniofacial issues, limb problems-in nearly 18% of exposed pregnancies. You must stop at least 3 months before trying to conceive.
- Mycophenolate mofetil (CellCept): Used for lupus nephritis. Linked to a 24% risk of birth defects, including ear and eye abnormalities. Stop at least 6 weeks before conception, but doctors recommend 3 months.
- JAK inhibitors (tofacitinib, upadacitinib): Still not well studied. EULAR and ACOG say avoid. Japan’s data is more lenient, but most U.S. doctors won’t risk it.
TNF Inhibitors: Which One Should You Pick?
If you’re on a TNF inhibitor, you’re not stuck with whatever you’re on. There’s a big difference between them.- Certolizumab pegol (Cimzia): Only 0.2% crosses the placenta. That’s why it’s the top choice for women in the third trimester. No need to stop before delivery.
- Adalimumab (Humira): About 15.7% crosses the placenta. Safe, but many doctors pause it after 30 weeks to reduce newborn exposure.
- Infliximab (Remicade): 23.4% crosses. Similar to adalimumab, but less commonly used now due to dosing.
- Etanercept (Enbrel): Around 10% crosses. Often paused after 30 weeks, but data is limited.
Biosimilars: Are They the Same?
Since Humira’s patent expired in early 2023, eight biosimilars hit the market-Amjevita, Hyrimoz, Hadlima, and others. You might wonder: are they safe during pregnancy? Yes. The FDA requires biosimilars to match their reference drug exactly in structure, function, and safety profile. If Humira is safe, so is Amjevita. No extra risk. No hidden differences. You can switch confidently if cost is a concern.What About Breastfeeding?
A lot of women worry about passing meds through breastmilk. The good news? Almost all biologics and DMARDs used for autoimmune disease have minimal transfer.- Hydroxychloroquine: Safe. Low levels in milk.
- Azathioprine: Safe. No reported issues in over 200 breastfed infants.
- TNF inhibitors: Less than 0.1% of maternal dose reaches milk. Babies absorb almost none.
- Methotrexate and mycophenolate: Still contraindicated during breastfeeding.
The Real Problem: Doctors Don’t Know Enough
Here’s the scary part: many OB-GYNs aren’t trained in autoimmune disease. They still think all immunosuppressants are dangerous. One study found that 68% of women with autoimmune conditions felt anxious about meds-and 42% stopped them without telling their doctor. That’s why you need a team. Not just an OB. Not just a rheumatologist. Both. The best outcomes come from preconception counseling with a rheumatologist who specializes in pregnancy and a maternal-fetal medicine specialist. At Duke’s pregnancy clinic, this approach cut unsafe medication use at conception from 39% to just 8%. Don’t wait for your first prenatal visit. Start 6 months before you try. Bring your full med list. Ask: Which ones do I need to switch? When? What’s the safest plan?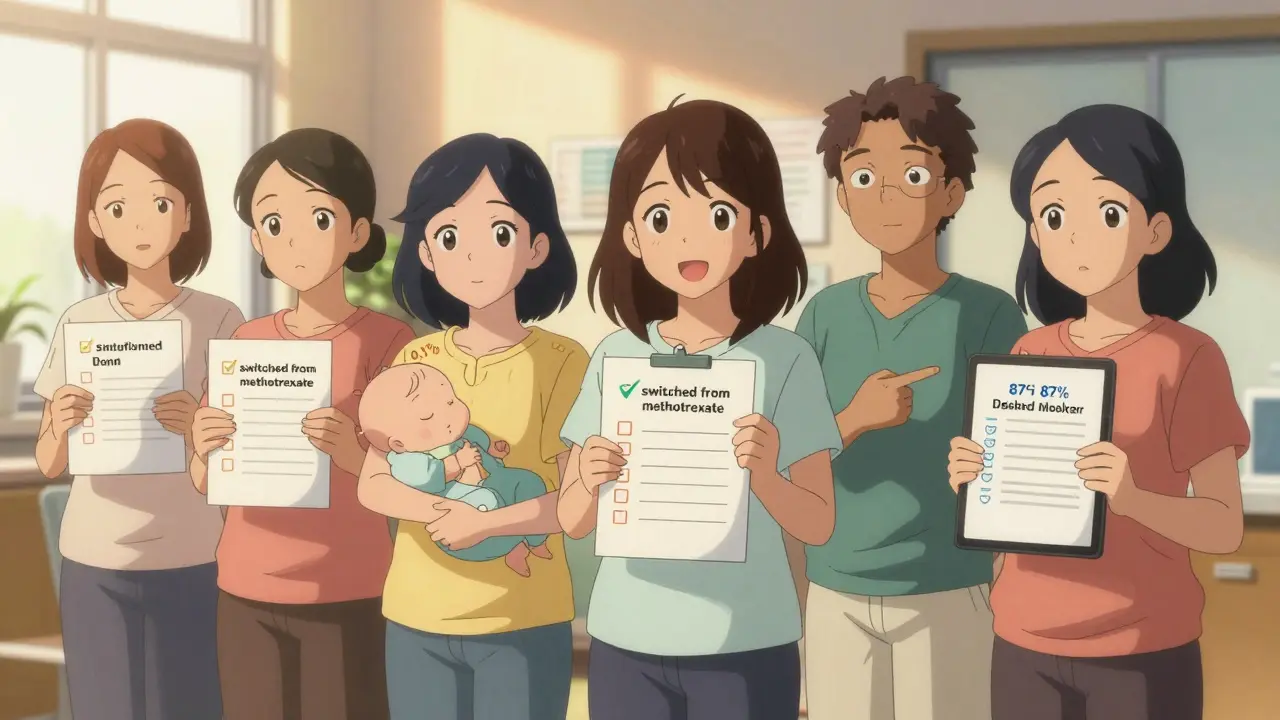
What’s New in 2025?
The field is moving fast. In February 2025, EULAR updated its guidelines based on over 1,200 studies. For the first time, they confirmed that 87% of standard treatments are safe during pregnancy and breastfeeding. ACOG is updating its 2019 guidelines in mid-2025 to match. The NIH just launched a $12.7 million research network to study newer drugs like JAK inhibitors in pregnancy. And by late 2025, we’ll have results from a major clinical trial on certolizumab in pregnancy. There’s also a new tool in development-a risk calculator that uses 12 factors (like your disease history, flare frequency, and lab results) to predict your chance of flaring during pregnancy. It’s 87% accurate. Soon, it’ll help you make decisions based on your body-not guesswork.Real Stories, Real Outcomes
One woman posted on a patient forum: "Continued hydroxychloroquine throughout pregnancy. Baby born at 39 weeks, 7 lbs 10 oz. Zero complications." Another: "Stopped adalimumab at 8 weeks because my OB said it was risky. Flared at 20 weeks. Needed prednisone. Got gestational diabetes. Delivered at 34 weeks." The difference? One followed evidence. The other followed fear.Your Action Plan
If you’re thinking about pregnancy, here’s what to do next:- Make an appointment with your rheumatologist now, even if you’re not trying yet.
- Ask: "Which of my meds are safe? Which ones need to change?" Bring a list.
- Request a referral to a maternal-fetal medicine specialist.
- If you’re on methotrexate or mycophenolate, start switching today. Give yourself 3-6 months.
- Don’t stop meds on your own. Flares hurt your baby more than most drugs.
- Keep taking hydroxychloroquine if you have lupus. It’s your best protection.
- Consider certolizumab if you’re on a TNF inhibitor and plan to carry past 30 weeks.
- Track your disease activity. Flares before pregnancy mean higher risks.
Final Thought: You Don’t Have to Choose
You don’t have to choose between being healthy and having a baby. That’s the myth. The truth is, with the right plan, you can do both. The science is clear. The tools are here. The experts are ready. What’s missing is the conversation. Start it. Before you get pregnant. Before the fear takes over. Before someone tells you to stop your meds. You deserve to feel safe. Your baby does too.Can I get pregnant if I have lupus or rheumatoid arthritis?
Yes, absolutely. Most women with autoimmune diseases can have healthy pregnancies. The key is planning. Disease activity matters more than the diagnosis itself. If your condition is well-controlled before conception, your chances of a healthy pregnancy are very high. Work with a rheumatologist and maternal-fetal medicine specialist at least 6 months before trying.
Is hydroxychloroquine safe during pregnancy?
Yes. Hydroxychloroquine is one of the safest autoimmune medications during pregnancy. It’s been studied in over 12,000 pregnancies with no increased risk of birth defects. For women with lupus, it reduces flares by 66% and cuts the risk of preeclampsia and preterm birth in half. It’s also safe while breastfeeding.
What happens if I stop my meds during pregnancy?
Stopping your medication without medical advice increases your risk of a disease flare by up to 63%. Flares during pregnancy raise the chance of preterm birth, preeclampsia, low birth weight, and even miscarriage. In most cases, the risks from uncontrolled disease are far greater than the risks from continuing safe medications like hydroxychloroquine, azathioprine, or certolizumab.
Are biologics like Humira safe during pregnancy?
Yes, TNF inhibitors like adalimumab (Humira), etanercept, and certolizumab pegol are considered safe during pregnancy. Over 28,000 documented pregnancies show no increase in major birth defects. Certolizumab pegol is preferred in the third trimester because it barely crosses the placenta. Most doctors pause adalimumab after 30 weeks, but it’s not required.
Can I breastfeed while on autoimmune meds?
Yes. Most medications used for autoimmune diseases-hydroxychloroquine, azathioprine, sulfasalazine, and all TNF inhibitors-transfer in negligible amounts to breastmilk. Studies show babies absorb less than 0.1% of the maternal dose. Breastfeeding is not only safe, it’s encouraged. Avoid methotrexate and mycophenolate while nursing.
When should I switch medications before pregnancy?
If you’re on methotrexate, stop at least 3 months before trying to conceive. For mycophenolate, stop at least 6 weeks before, but 3 months is safer. Switching to pregnancy-safe alternatives like hydroxychloroquine or azathioprine should start 3-6 months before conception. This gives your body time to clear the unsafe drugs and stabilize on the new ones.
Are biosimilars safe during pregnancy?
Yes. Biosimilars like Amjevita, Hyrimoz, and Hadlima are exact copies of their reference drugs (like Humira) in structure, function, and safety. The FDA requires them to match the original in all aspects, including pregnancy safety. If Humira is safe, so is its biosimilar.
Why do some doctors still say to stop all meds during pregnancy?
Many OB-GYNs aren’t trained in autoimmune disease. Their training often relies on outdated guidelines from 10-15 years ago, when the default advice was to stop everything. New research shows that’s wrong. The latest EULAR and ACOG guidelines (2024-2025) confirm most medications are safe. Always ask for a second opinion from a rheumatologist who specializes in pregnancy.
What’s the biggest mistake women make?
The biggest mistake is stopping medication on their own out of fear. Nearly 42% of women with autoimmune disease stop their meds without talking to a doctor. This leads to flares, which are far more dangerous to pregnancy than the medications themselves. The safest choice is often to stay on your proven, pregnancy-safe drug-not to stop it.
Is there a new tool to predict pregnancy risks?
Yes. A validated prediction tool developed by Dr. Megan Clowse’s team uses 12 clinical factors-like disease duration, flare frequency, lab markers, and medication history-to estimate your personal risk of flaring during pregnancy. It’s 87% accurate and will soon be available to help guide treatment decisions before conception.


Lawrence Jung
January 11, 2026 AT 18:59People still think meds are the enemy like its 2005
Stop being scared of science and start being scared of flares
Hydroxychloroquine saved my pregnancy and nobody told me it was safe until I found this post
Doctors are still stuck in the dark ages
Alice Elanora Shepherd
January 12, 2026 AT 05:48Thank you for this comprehensive, evidence-based overview-this is exactly the kind of clarity that’s so desperately needed.
Many women are terrified into stopping essential medications, often without consulting specialists, and the consequences can be devastating.
It’s reassuring to see that hydroxychloroquine, azathioprine, and certolizumab pegol have such robust safety data-especially in breastfeeding.
I’ve shared this with my rheumatology support group, and several members have already scheduled preconception consults.
Let’s keep pushing for better education among OB-GYNs, too-they’re often the first point of contact, and outdated beliefs persist.
Thank you again for demystifying what should be routine knowledge.
It’s not about avoiding medication-it’s about choosing wisely.
Christina Widodo
January 13, 2026 AT 05:52Wait so I can keep my Humira and still breastfeed??
My OB told me to stop at 20 weeks and I did and I flared so bad I cried for weeks
Why didn’t anyone tell me this before??
Also why is certolizumab not talked about more??
Is it harder to get or just not marketed?
Also is there a list of docs who actually know this stuff??
Like I don’t want to go to some random rheum who’s never heard of certolizumab
Also I’m trying again next month and I’m terrified I’ll mess up again
Jennifer Phelps
January 14, 2026 AT 05:55My doctor told me to stop everything and I did and I got preeclampsia at 28 weeks
My baby was in NICU for a month
Turns out I should’ve stayed on hydroxychloroquine
Now I’m trying again and I’m bringing this post to every appointment
Why is this not standard info??
Why do we have to Google this ourselves??
Someone needs to make a pamphlet for OB offices
Craig Wright
January 15, 2026 AT 20:39It is deeply concerning that such a fundamental matter of maternal health is left to the whims of patient self-education.
One would expect national health institutions to disseminate such critical guidance uniformly.
The fact that this information is scattered across forums and blogs reflects a systemic failure in public health communication.
Moreover, the reliance on American guidelines is somewhat parochial-European protocols differ in subtle but important ways.
One must question the adequacy of a system that leaves women to navigate life-altering medical decisions on Reddit.
Eileen Reilly
January 17, 2026 AT 04:32so like… if you’re on methotrexate and you get pregnant by accident… do you just abort??
or is it like… ‘oops’ and you keep going??
my cousin did that and now her kid has a weird hand thing
but like… is it 100% guaranteed to be a disaster??
or is there a chance??
also i heard you can just take folic acid and it fixes everything??
is that true??
plz halp
Monica Puglia
January 18, 2026 AT 09:25THIS. IS. EVERYTHING. 🙌
My rheum just said ‘oh we’ll figure it out when you get pregnant’
NO. WE ARE FIGURING IT OUT NOW. 🧠
Just started switching from methotrexate to azathioprine and I feel like I just got my power back
Also breastfeeding with TNF inhibitors?? YES PLEASE 🤱
Why is this not on every OB’s website??
Also if you’re reading this and you’re scared… you’re not alone. I was too. But knowledge is power. 💪❤️
steve ker
January 20, 2026 AT 00:10So you’re telling me the West has been lying to women for decades?
And now you want us to trust doctors again?
Pathetic.
Just have the baby.
Let nature take its course.
Medications are for weak people.
End of story.
George Bridges
January 21, 2026 AT 13:01I’m a guy and I don’t have an autoimmune disease but my wife does.
This post changed everything for us.
We had no idea so much was known, so much was safe.
She was ready to give up on having kids because everyone told her it was too risky.
Now she’s talking to her rheum next week and we’re both actually hopeful for the first time.
Thank you for writing this.
It’s not just medical info.
It’s hope.
Faith Wright
January 23, 2026 AT 01:07Oh so now we’re supposed to trust Big Pharma’s ‘safe’ meds?
But the FDA is just a revolving door for pharma execs
And you think hydroxychloroquine is safe because 12,000 women took it?
Where’s the long-term data on the kids??
What about epigenetics??
And why is certolizumab the ‘safest’? Because it’s the most expensive?
Classic corporate medicine.
But hey, keep taking your pills.
I’m sure your kid will be fine… probably.
Rebekah Cobbson
January 24, 2026 AT 02:58Okay I just got off the phone with my rheum and we switched me from methotrexate to azathioprine
And I cried because I finally feel like someone gets it
Also I asked about certolizumab and she said ‘yes, that’s the one I recommend for third trimester’
So I’m doing it
And I’m telling every other woman I know
Because this isn’t just about meds
It’s about being allowed to be a mom without guilt
You don’t have to choose
And you don’t have to suffer in silence
Thank you for writing this
It saved me
Audu ikhlas
January 25, 2026 AT 14:00Y’all are too soft
In Nigeria we just take herbs and pray
Why you need all these pills?
God will protect
And if baby die? God will give another
Why you waste money on American drugs?
My cousin had 7 kids with lupus
Only 4 survive
But they strong
You need less science
More faith
And less typing on phone