SSRI Dose Adjustment Calculator
This calculator helps estimate appropriate SSRI dosing based on your CYP2C19 or CYP2D6 metabolic status. Results are for informational purposes only and should not replace professional medical advice.
Choosing the right SSRI shouldn’t feel like rolling dice. You take the medication, wait weeks for it to work, and hope you don’t end up with nausea, dizziness, or insomnia-side effects that make people quit before they even give it a real shot. For many, this isn’t bad luck. It’s genetics.
Why Your Body Processes SSRIs Differently
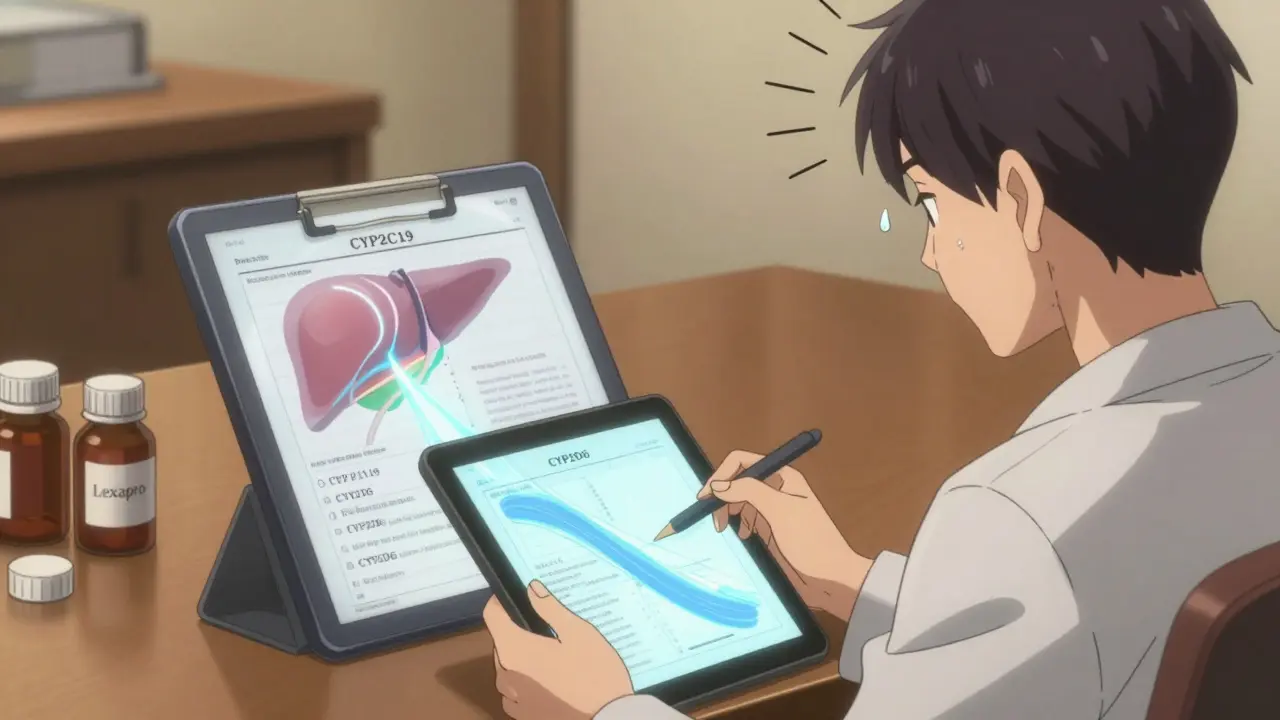
Your liver has enzymes that break down medications, and two of the most important ones are coded by genes called CYP2C19 and CYP2D6. These aren’t just random proteins-they’re your body’s chemical factories for antidepressants. If your version of these genes works slowly, you’ll have too much drug building up in your system. If they work too fast, the drug gets cleared before it can help.That’s why two people on the same dose of escitalopram (Lexapro) can have wildly different experiences. One feels calmer after two weeks. The other feels sick and stops taking it. The difference? Their genes.
Studies show that people with a poor metabolizer version of CYP2C19 have 2.3 to 3.5 times higher levels of escitalopram in their blood than normal metabolizers. That’s not a small difference-it’s enough to push someone into side effect territory. The same goes for CYP2D6 and drugs like paroxetine (Paxil) and venlafaxine (Effexor). Poor metabolizers here are 2.7 times more likely to report severe dizziness or nausea.
What the Test Actually Measures
Pharmacogenomic testing doesn’t look at your whole genome. It focuses on specific variants in CYP2C19 and CYP2D6 that change how fast you process SSRIs. There are four main categories of metabolism:- Poor metabolizer (PM): Enzymes barely work. High risk of side effects.
- Intermediate metabolizer (IM): Slower than average. May need lower doses.
- Normal metabolizer (NM): Standard processing. Standard dose usually works.
- Ultrarapid metabolizer (UM): Enzymes work too fast. Drug gets cleared before it helps.
CYP2C19 adds a fifth group: rapid metabolizer (RM), which behaves similarly to ultrarapid but is less extreme. These labels aren’t guesses-they’re based on combinations of known genetic variants, called star alleles. For example, CYP2D6*4 and *5 are common poor metabolizer variants in people of European descent. CYP2C19*2 and *3 are the most frequent loss-of-function variants globally.
Testing is done with a simple cheek swab or blood sample. Labs use targeted arrays or sequencing to catch the tricky variants that standard DNA tests miss-especially with CYP2D6, which has a confusing pseudogene that can throw off results if not tested properly. Accuracy? Around 95-99% when done right.
Which SSRIs Are Affected?
Not all antidepressants are equal when it comes to these genes. Here’s what you need to know:| Antidepressant | Primary Enzyme | Common Brand Names |
|---|---|---|
| Citalopram | CYP2C19 | Celexa |
| Escitalopram | CYP2C19 | Lexapro |
| Sertraline | CYP2C19 | Zoloft |
| Fluoxetine | CYP2D6 | Prozac |
| Paroxetine | CYP2D6 | Paxil |
| Fluvoxamine | CYP2D6 | Luvox |
| Venlafaxine | CYP2D6 | Effexor XR |
If you’re prescribed one of these, your CYP2C19 or CYP2D6 status can make or break your treatment. For example, a CYP2C19 poor metabolizer on citalopram might need half the dose to avoid QT prolongation-a heart rhythm issue that can be dangerous. A CYP2D6 ultrarapid metabolizer on paroxetine might never feel any benefit because the drug vanishes before it can act.
What the Evidence Really Says
Let’s cut through the noise. Yes, pharmacogenomic testing shows clear differences in drug levels. But does that always mean better outcomes?A 2024 study of over 5,800 people found no strong link between CYP2C19 genotype and whether escitalopram worked-only how much of it stayed in their blood. That’s the big gap: pharmacokinetics (what your body does to the drug) doesn’t always match pharmacodynamics (what the drug does to your brain).
But here’s where it matters: side effects. The data is solid. A 2023 case series described a woman on venlafaxine who developed crippling dizziness at 75 mg. Her test showed she was a CYP2D6 poor metabolizer. Dropping her dose to 37.5 mg eliminated the side effects-and she stayed on treatment. Another patient, an ultrarapid metabolizer, didn’t respond to 20 mg of escitalopram. Doubling the dose to 40 mg worked. That’s not theory. That’s real life.
And the numbers back it up. Patients with poor metabolizer status were 3.2 times more likely to report severe side effects with paroxetine. For citalopram, the risk was 2.8 times higher. These aren’t rare outliers. They’re predictable outcomes based on biology.
Who Benefits Most?
This isn’t for everyone. If you’ve tried one SSRI, had mild side effects, and it worked-great. You probably don’t need this test.But if you’ve:
- Failed two or more antidepressants due to side effects
- Had a bad reaction to a low dose
- Been told you’re "treatment-resistant"
- Have a family history of bad reactions to psychiatric meds
-then this test could save you months of trial and error. One 2022 analysis found that using pharmacogenomic testing could save $1,200 to $1,800 per patient by avoiding ineffective prescriptions and ER visits for side effects.
It’s also valuable for older adults, people taking multiple meds, or those with liver issues. These groups are more vulnerable to drug buildup, and genetics can explain why.
What’s Holding It Back?
The science is strong. So why isn’t every psychiatrist ordering this test?Insurance coverage is spotty. Only 62% of U.S. insurers cover it for antidepressants as of mid-2024. In Australia, Medicare doesn’t fund it yet, though private insurers sometimes do. Out-of-pocket cost? Around $300-$500.
Interpretation is tricky. A single gene result isn’t enough. What if you’re a CYP2C19 poor metabolizer but also take a CYP2D6 inhibitor like fluoxetine? The interaction can turn a normal metabolizer into a poor one. That’s why experts recommend using CPIC’s free online dosing tools or consulting a pharmacogenomics-certified pharmacist. There are about 1,200 in the U.S. alone.
And some doctors still don’t trust it. A 2023 editorial in JAMA Psychiatry warned that genetics is just one piece of the puzzle. Depression isn’t just about enzymes-it’s about stress, sleep, trauma, inflammation, and more. Testing won’t fix all that.
What’s Next?
The field is moving fast. The latest CPIC guidelines (April 2023) now include four more genes beyond CYP2C19 and CYP2D6-like SLC6A4 and HTR2A-that influence serotonin transport and receptor sensitivity. That means future tests will give a fuller picture.The NIH just launched GUIDED-2, a $15.2 million study tracking 5,000 people with treatment-resistant depression. Results by 2027 could finally prove whether this testing leads to better recovery rates-not just fewer side effects.
Meanwhile, some clinics are already using polygenic risk scores that combine genetics with clinical factors like age, weight, and comorbidities. By 2026, this could become standard in major hospitals.
Should You Get Tested?
If you’ve struggled with SSRIs before, yes. It’s not magic. It won’t guarantee you’ll feel better. But it removes guesswork. Instead of trying five drugs over two years, you might get it right on the second try.Start by asking your doctor if they’ve used pharmacogenomic testing before. If they haven’t, ask if they’re willing to review CPIC guidelines or consult a clinical pharmacist. Some labs offer direct-to-consumer tests, but make sure they’re CLIA-certified and provide clinician support for interpretation.
This isn’t about replacing your doctor. It’s about giving them better tools to help you.
Is pharmacogenomic testing covered by insurance?
Coverage varies. In the U.S., about 62% of major insurers cover CYP2C19 and CYP2D6 testing for antidepressants as of 2024. Medicare and Medicaid typically don’t cover it yet. In Australia, private health insurers sometimes cover it under extras, but Medicare does not. Always check with your provider before ordering.
How long does it take to get results?
Most labs take 1 to 3 weeks from the time you submit your sample. Some offer expedited services for an extra fee, but standard turnaround is usually around 14 days. Your doctor will typically schedule a follow-up to discuss results and adjust your medication if needed.
Can I get tested without seeing a doctor?
Yes, some companies sell direct-to-consumer tests online. But without a clinician to interpret the results in context of your full medical history, you risk misusing the information. For example, a poor metabolizer might stop their SSRI entirely instead of lowering the dose. Always work with a provider who understands pharmacogenomics.
Does this test work for all antidepressants?
No. It’s most reliable for SSRIs and tricyclic antidepressants metabolized by CYP2C19 and CYP2D6, like escitalopram, sertraline, paroxetine, and venlafaxine. It’s less useful for drugs like bupropion, mirtazapine, or SNRIs like desvenlafaxine, which use different metabolic pathways.
If I test as a poor metabolizer, do I have to avoid SSRIs entirely?
No. You don’t avoid them-you adjust. For CYP2C19 poor metabolizers, doctors often reduce the dose of citalopram or escitalopram by 50%. For CYP2D6 poor metabolizers, switching to an SSRI that doesn’t rely on that enzyme-like sertraline or fluoxetine-can help. The goal is personalized dosing, not elimination.
Is this test worth it if I’ve never had side effects?
Probably not. If your current SSRI is working well with minimal side effects, there’s little benefit to testing. The real value is for people who’ve had repeated failures or bad reactions. It’s a tool for troubleshooting-not a routine screening.


Alex Danner
January 6, 2026 AT 16:51Finally, someone broke this down without the corporate fluff. I had to try four SSRIs before my doc ordered the test. Turned out I’m a CYP2D6 poor metabolizer. Paroxetine made me feel like I was walking through molasses. Cut the dose in half? Suddenly I could sleep, work, and not cry in the shower. This isn’t sci-fi-it’s biology.
Doctors still act like genetics is optional. It’s not. Your liver doesn’t care what your insurance says.
Rachel Steward
January 8, 2026 AT 08:24Let’s be real-this test is just another way for labs to make money while doctors outsource their critical thinking. Sure, your enzymes might be slow, but depression isn’t a chemistry set. Trauma, poverty, sleep deprivation, loneliness-none of that shows up in a cheek swab. You think your genes are the problem? Maybe your life is.
And don’t get me started on ‘ultrarapid metabolizers.’ That’s just a fancy way of saying ‘your body hates antidepressants.’ Congrats, you’re genetically unlucky. Now what? Pay $500 to hear the same thing your grandma told you: ‘Try harder.’
steve rumsford
January 10, 2026 AT 01:26my doc tried to push me on lexapro even after i told her i got nauseous on it before. i was like bro i dont need a gene test to know my body says no. she said 'but the science says...' and i said 'the science also said thalidomide was safe.'
point is, if you feel like crap on a drug, stop taking it. dont wait for a lab report. your body talks. listen.
also cyp2c19? sounds like a spaceship engine.
Katrina Morris
January 11, 2026 AT 01:21as someone from the midwest where mental health care is a luxury i just want to say thank you for writing this without jargon
my cousin took zoloft for 3 years and never got better until she switched to sertraline after testing showed she was a poor metabolizer on cyp2c19
she said it felt like someone turned on the lights in her brain
if this helps even one person avoid years of suffering its worth it
ps i spelled cyp wrong three times but you know what i mean
LALITA KUDIYA
January 12, 2026 AT 20:36in india we dont even have access to these tests but i still read everything i can
my mom took paroxetine and got so dizzy she fell down the stairs
the doctor said she was 'overthinking' but now i know it was her genes
thank you for sharing this
❤️
Poppy Newman
January 14, 2026 AT 07:41OMG this is so important 😭 I’ve been on 7 antidepressants and every time it’s ‘maybe try a higher dose’ or ‘give it more time’… what if the problem isn’t time or dose but my liver just… doesn’t wanna?
Just got my test results last week-CYP2C19 poor metabolizer. Switched from escitalopram to sertraline. Two weeks in and I’m actually smiling again. Not ‘trying to smile’-actual smiling.
Why isn’t this standard??
Jessie Ann Lambrecht
January 15, 2026 AT 12:36Let me tell you about my friend who’s a CYP2D6 ultrarapid metabolizer. She was on 150mg of venlafaxine and felt nothing. Zero. Nada. Her therapist called her ‘resistant.’ Turns out her body was flushing the drug out faster than her coffee machine brews espresso.
Doubled the dose to 300mg? Boom. Relief. No more crying in the parking lot before work.
This isn’t ‘alternative medicine.’ It’s precision medicine. And if your doctor acts like it’s witchcraft, find a new one. You deserve better than trial-by-error.
Also-sertraline is your BFF if you’re CYP2C19 impaired. Don’t let them push you into citalopram unless you want to feel like a zombie with a side of heart palpitations.
Kyle King
January 15, 2026 AT 13:29fake science. big pharma and gene labs are in bed together. they want you to think your depression is in your DNA so you’ll keep buying pills and never question why you’re depressed in the first place.
you think your genes are the problem? check your job. your rent. your loneliness. your trauma. your soul.
they’ll sell you a $500 swab to avoid fixing capitalism.
also cyp2d6? sounds like a government surveillance program.
Kamlesh Chauhan
January 16, 2026 AT 04:06why are we even doing this
you take a pill you feel bad you take another pill
why not just go outside and touch grass
or cry in a room
or drink tea
why do we need labs and genes and charts
its all just corporate nonsense
and the test costs 500 bucks
what if i dont have 500 bucks
what if i just need someone to listen
Mina Murray
January 16, 2026 AT 08:26So you’re telling me we’re now reducing complex psychiatric conditions to single-gene polymorphisms? Brilliant. Next they’ll test for ‘sadness alleles’ and charge extra for the ‘happy variant’ upgrade.
And let’s not forget-this test doesn’t account for drug interactions. You’re a poor metabolizer on CYP2C19 but also on fluoxetine? Congrats, you just turned yourself into a walking drug overdose waiting to happen.
Doctors who blindly trust this are playing Russian roulette with people’s lives. And don’t get me started on direct-to-consumer kits. People are self-prescribing based on a PDF from a lab that doesn’t even require a license.
This isn’t medicine. It’s genetic astrology.
Jonathan Larson
January 17, 2026 AT 12:07As a clinician with over 15 years in psychiatric care, I can attest to the transformative impact of pharmacogenomic testing in select populations. The data is not merely statistically significant-it is clinically meaningful. We have seen patients who had been institutionalized due to treatment-resistant depression achieve functional recovery after genotype-guided dosing.
It is not a panacea. It is not a replacement for psychotherapy, social support, or lifestyle interventions. But when integrated thoughtfully into a biopsychosocial model, it reduces suffering, accelerates remission, and restores dignity.
To those who dismiss it as reductionist: consider this-would you refuse a blood test for diabetes because ‘stress causes high sugar’? Precision is not simplification. It is liberation from guesswork.
Andrew N
January 18, 2026 AT 17:02the study said no link between gene and effectiveness
so why are we even talking about this
side effects? yeah sure
but if the drug doesn’t work anyway
what’s the point
just take whatever your doc gives you
or don’t take anything
either way you’re gonna feel like crap
Alex Danner
January 19, 2026 AT 08:47Andrew N, you’re missing the point. The study didn’t say the gene doesn’t affect outcomes-it said it doesn’t predict if the drug ‘works’ for depression. But side effects? That’s where it matters. If you’re too sick to even try therapy or go to work, does it matter if the drug ‘works’? You’re not treating depression-you’re treating survival.
My cousin was a CYP2D6 poor metabolizer. She couldn’t leave her bed at 75mg of venlafaxine. Cut it to 37.5mg? She started walking again. That’s not ‘effectiveness.’ That’s being human.