Why Your Bones Are Weakening Faster Than You Think
By age 50, 1 in 3 women and 1 in 5 men will break a bone because of weak bones. Not from a car crash or sports injury - but from something as simple as tripping on a rug or coughing too hard. This isn’t aging. This is osteoporosis - a silent disease that eats away at your bones without warning.
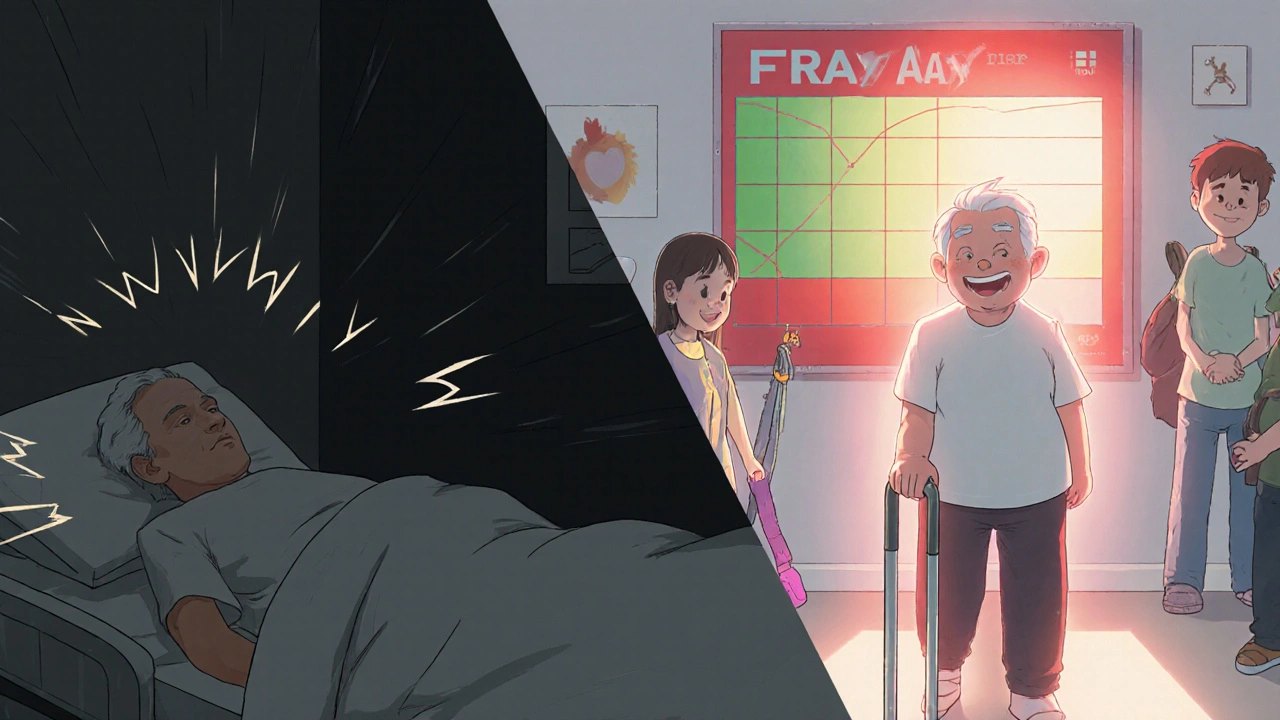
Most people don’t know they have it until they fall. And when they do, the consequences are serious. About 1 in 5 people who break a hip won’t survive the next year. Others lose their independence, end up in nursing homes, or live in constant pain. The good news? You can stop this. Not with magic pills, but with real, daily actions that work - if you start now.
What’s Actually Harming Your Bones?
Your bones aren’t just passive structures. They’re alive, constantly being rebuilt. But when the body breaks down bone faster than it rebuilds it, you lose density. That’s osteoporosis.
Some things you can’t change. Being a woman over 50? Higher risk. Being over 65? Risk jumps again. Having a parent who broke a hip? Your risk goes up by 60-80%. Being Asian or White? You’re more likely to develop it than Black or Hispanic people.
But here’s the truth: most of your risk is in your control. And it’s not just about calcium.
The Real Culprits Behind Bone Loss
Low calcium? Yes, that matters. But you need more than milk. Most adults need 1,000-1,200 mg a day. That’s about 3 servings of dairy, or 4 cups of fortified plant milk, plus leafy greens. If you’re not hitting that, you’re falling behind.
Vitamin D is just as critical. Without it, your body can’t absorb calcium. Over 40% of adults in the U.S. are deficient. If your levels are below 20 ng/mL, your fracture risk goes up by 33%. You don’t need a lab test to fix this - 800-1,000 IU of vitamin D daily will do it for most people. If you’re deficient, 2,000 IU for a few months can bring you back up.
Smoking? It cuts calcium absorption and lowers estrogen. One pack a day increases fracture risk by 55%. Alcohol? More than two drinks a day raises your hip fracture risk by 41%. And sitting all day? That’s like telling your bones to stop growing. Sedentary people have 25-30% higher fracture risk.
Some meds wreck your bones too. Long-term steroid use - even for asthma or arthritis - can zap 5-15% of your bone density in just one year. That’s faster than natural aging. If you’re on steroids, talk to your doctor about bone protection.
Fracture History Is the Biggest Warning Sign
Here’s something most doctors don’t stress enough: if you’ve already broken a bone from a minor fall, your chance of breaking another skyrockets. A spine fracture? Your risk of another goes up by 86%. A hip fracture? Up by 200%.
That’s more powerful than any scan. Your bone density score (T-score) might say “osteopenia,” but if you’ve fractured before, you’re already in the danger zone. Dr. Ethel Siris, a leading bone specialist, says: “A single fragility fracture doubles your risk of another - more than low bone density alone.”
Don’t wait for a DXA scan to act. If you’ve fallen and cracked a rib, wrist, or spine - even if it didn’t hurt badly - get checked. Your next fracture could be worse.

What Actually Builds Bone? (It’s Not Just Calcium Pills)
Exercise isn’t just for your heart. It’s your bones’ best friend.
Weight-bearing activity - walking, hiking, stair climbing, dancing - tells your bones: “Stay strong.” Resistance training - lifting weights, using resistance bands - is even better. A 2023 Yale study found people who did 5 days a week of walking and 2 days of lifting reduced fracture risk by 30-40%.
You don’t need a gym. Try this: walk 30 minutes most days. Do 10 squats, 10 heel raises, and 10 wall push-ups every morning. Hold onto a chair if you need to. Do it for 6 months, and your bones will respond.
Balance training matters too. Falls cause 90% of fractures. Tai Chi, yoga, or simple balance drills - standing on one foot while brushing your teeth - cut falls by 45%. That’s huge.
When to Get Tested - And What the Numbers Mean
The DXA scan is the gold standard. It’s quick, safe (less radiation than a flight from Perth to Sydney), and tells you exactly where you stand.
Recommendations: Women over 65. Men over 70. Anyone over 50 who’s had a fracture, is on steroids, or has a family history.
Your T-score tells the story:
- ≥ -1.0: Normal bone density
- -1.0 to -2.5: Osteopenia (low bone mass - not osteoporosis yet)
- ≤ -2.5: Osteoporosis
But here’s the catch: half the people who fracture have T-scores in the osteopenia range. That’s why doctors now use FRAX - a tool that combines your age, sex, weight, smoking status, alcohol use, and fracture history to calculate your 10-year fracture risk. If it’s over 20%, treatment is usually recommended - even if your bone density isn’t “bad.”
Medications: Helpful, But Not a Fix-All
Drugs like alendronate (Fosamax) or romosozumab (Evenity) can help. Evenity, approved in 2023, actually builds new bone while slowing loss - a rare combo. It cuts spine fractures by 73% in a year.
But they’re not for everyone. Many people stop taking them because of stomach upset, jaw pain, or muscle aches. One study found 38% quit within a year. If a drug makes you feel worse, talk to your doctor. There are alternatives - even injectables that only come once every 6 months.
Medication works best with lifestyle changes. No pill can undo years of inactivity or poor nutrition.
What Really Works in Real Life
People who stick with prevention don’t do it perfectly. They just do it consistently.
One woman in Perth, 68, started walking her dog every morning and did 10 squats while waiting for the kettle to boil. After 8 months, her balance improved. She hasn’t fallen since.
A man in his 70s switched from soda to fortified orange juice and added two eggs a day. He raised his vitamin D and protein intake - two things he didn’t realize were hurting his bones.
Another group in a UK trial did supervised exercise for 6 months. They reported better confidence, less fear of falling, and 45% fewer falls. No drugs. Just movement.
It’s not about being perfect. It’s about showing up.
Make Your Home Safe - Before You Fall
Fractures don’t happen in gyms. They happen at home.
- Remove loose rugs or tape them down.
- Install grab bars in the shower and next to the toilet.
- Keep floors clear - shoes, cords, toys.
- Use nightlights in hallways and bathrooms.
- Get non-slip mats in the tub.
- Make sure stairs have sturdy handrails on both sides.
These aren’t “old person” fixes. They’re smart safety moves for anyone over 50 - especially if you’ve had a fall before.
Start Now - Before It’s Too Late
Peak bone mass is built by age 30. But your bones never stop listening. Even at 60, 70, or 80, they respond to movement, nutrition, and safety.
You don’t need a perfect diet. Just more calcium-rich foods. You don’t need to run marathons. Just walk more. You don’t need to take every supplement. Just get your vitamin D checked.
The biggest mistake? Waiting for a fracture to wake you up. By then, it’s too late to prevent the next one.
Today, do one thing: walk for 20 minutes. Eat a yogurt or a handful of almonds. Stand on one foot while brushing your teeth. Tell someone you’re taking your bone health seriously.
That’s how you stop osteoporosis before it stops you.
Can osteoporosis be reversed?
You can’t fully restore bone density to what it was at age 25, but you can stop further loss and even rebuild some density - especially with medications like romosozumab and consistent weight-bearing exercise. Many people improve their T-score by 1-2 points over 1-2 years with the right combination of movement, nutrition, and treatment.
Do I need to take calcium supplements?
Not always. If you eat 3 servings of calcium-rich foods daily - like dairy, fortified plant milks, tofu, sardines, or leafy greens - you may not need a supplement. But most people fall short. If your diet is low, take 500-600 mg of calcium with meals (your body absorbs it better that way). Don’t take more than 1,200 mg total per day from all sources - too much can raise heart risk.
Is walking enough to strengthen bones?
Walking helps - but it’s not enough on its own. For bone strength, you need impact (like brisk walking or stair climbing) and resistance (like lifting weights or using bands). Walking 5 days a week plus 2 days of light strength training is the sweet spot. Just strolling the neighborhood won’t cut it if you’re trying to rebuild bone.
What’s the best time of day to get vitamin D?
Sunlight is the best natural source, but in Perth, even in winter, 10-15 minutes of midday sun on your arms and face 3-4 times a week is usually enough. But if you’re over 50, have dark skin, or stay indoors - you likely need a supplement. Take it with a meal that has fat (like avocado or nuts) for better absorption. Time of day doesn’t matter much for pills - consistency does.
Can I still exercise if I have osteoporosis?
Yes - and you should. But avoid high-impact activities like jumping, heavy lifting with poor form, or deep forward bends (like toe touches). Focus on safe weight-bearing walks, resistance training with light weights, and balance exercises. A physiotherapist who specializes in bone health can design a program that keeps you strong without risking a fracture.
Are men really at risk for osteoporosis?
Absolutely. 1 in 5 men over 50 will break a bone due to osteoporosis. Men often ignore it because it’s seen as a “woman’s disease.” But men lose bone too - especially after 70, or if they’re on steroids, have low testosterone, smoke, or drink heavily. Men are also more likely to die after a hip fracture than women. Don’t assume you’re safe.
How long does it take to see results from bone-healthy habits?
Bone changes slowly. You won’t feel stronger right away. But after 6-12 months of consistent exercise and good nutrition, your bone density may start to improve. Balance and confidence improve faster - often in 3-4 months. The goal isn’t instant results. It’s long-term protection. Every day you choose movement over sitting, you’re lowering your fracture risk.
What foods are best for bone health?
Focus on calcium, vitamin D, protein, and magnesium. Good sources: dairy (milk, yogurt, cheese), fortified plant milks, canned sardines or salmon with bones, tofu made with calcium sulfate, kale, bok choy, almonds, and Brazil nuts. Protein is critical too - aim for 1.0-1.2 grams per kg of body weight. A 70kg person needs about 70-85g of protein daily - that’s 2-3 palm-sized portions of meat, fish, eggs, or legumes.


Shawn Sakura
November 20, 2025 AT 21:00Yo, this hit different. I’m 62 and just started doing squats while waiting for my coffee-no gym, no fancy gear. My balance is way better, and I haven’t tripped over my own feet in 4 months. 🙌 Also, switched from soda to fortified OJ. My doc said my vit D jumped from 18 to 34. Small stuff, y’all. Small stuff.
Elaina Cronin
November 22, 2025 AT 10:02While I appreciate the practical advice, I must emphasize that the underlying assumption-that individual behavioral change alone can counteract decades of systemic neglect in public health infrastructure-is dangerously naive. Bone density loss is not merely a matter of diet or walking; it is a consequence of pharmaceutical lobbying, inadequate Medicare coverage for preventive care, and the commodification of wellness. Without structural reform, your yoga mats and almond milk are Band-Aids on a hemorrhage.
Willie Doherty
November 23, 2025 AT 18:04As a clinical epidemiologist with 22 years in bone health research, I must correct a critical misstatement: the claim that ‘1 in 5 men over 50 will break a bone due to osteoporosis’ is misleading. The true incidence is closer to 1 in 8 when adjusted for comorbidities and fracture mechanism. The 1 in 5 figure conflates all fragility fractures with osteoporosis-specific etiology. Misrepresentation of this nature erodes public trust in evidence-based medicine.
Cooper Long
November 25, 2025 AT 08:52Protein intake recommendation is accurate. 1.0–1.2g/kg is optimal. However, the emphasis on dairy is outdated. Many populations thrive on plant-based calcium sources without dairy. Cultural context matters. Also, vitamin D supplementation should be individualized based on serum levels-not blanket 800–1000 IU. One size does not fit all.
Paula Jane Butterfield
November 25, 2025 AT 10:23My mom is 74 and just started walking with her grandkids after school. She does 10 heel raises while brushing her teeth and uses a resistance band while watching TV. She didn’t even know she had osteopenia until her hip hurt last year. Now she says she feels ‘like she’s got roots.’ No meds. Just consistency. If she can do it, we all can. 💪
David Cusack
November 25, 2025 AT 15:34...and yet, the author neglects to mention the role of phthalates in bone metabolism...the endocrine disruptors in plastic food containers...the subtle, insidious erosion of bone integrity by industrialized food systems...and here we are, lecturing about yogurt...as if the problem lies in our laziness...not in the poisoned well from which our sustenance flows...
Darragh McNulty
November 25, 2025 AT 22:40THIS. I’m 69 and did exactly what the Perth woman did-walk the dog, squat while the kettle boils. Now I can climb stairs without wheezing. And I started doing one-foot stands while brushing my teeth. My wife says I look like a flamingo with a toothbrush 😆 But no falls. No fear. Just me, my dog, and my bones saying ‘thank you.’
Logan Romine
November 26, 2025 AT 05:12So let me get this straight… we’re supposed to believe that standing on one foot while brushing my teeth is the antidote to decades of industrial decline, pharmaceutical greed, and the slow death of the human skeleton? I mean… sure. I’ll just do my squats and hope the FDA doesn’t poison my calcium next. 🤡
Sandi Moon
November 27, 2025 AT 09:13Let’s not forget: DXA scans are unreliable. They measure density, not quality. Bone is not concrete. It’s a living lattice-microarchitecture matters. The FRAX tool? A corporate algorithm designed to sell drugs. The real solution? Stop eating processed food. Stop sitting. Stop trusting institutions. And for heaven’s sake, stop drinking fluoride-laced water.
Sheldon Bazinga
November 27, 2025 AT 23:43Bro. Bone health? You think this is about calcium? Nah. It’s about being a real American. You wanna not break your hip? Stop being weak. Lift real weights. Eat real meat. Stop drinking almond milk like a vegan hippie. And if you’re on steroids? Then you probably deserve to break your spine. Get tough. Or get a walker. 🇺🇸
Kartik Singhal
November 29, 2025 AT 00:48Interesting. But why no mention of 5G radiation? Or EMF exposure from smart meters? Or the fact that modern vitamin D supplements are often synthetic and bio-unavailable? The real issue is not diet-it’s the hidden toxins in our environment. And yet, the narrative remains simplistic. Classic. 🌐🧠