More than half of all new cancer drugs approved in the last five years come as pills you take at home. That’s not a convenience-it’s a responsibility. Oral chemotherapy gives you back time: no more weekly clinic visits, no IV needles, fewer disruptions to your life. But here’s the truth no one tells you upfront: oral chemotherapy is only as effective as the dose you actually take. Miss one pill. Take it with the wrong food. Store it wrong. And you could be sabotaging your treatment without even knowing it.
How Oral Chemotherapy Works-And Why It’s Different
Oral chemotherapy isn’t just IV chemo in a pill. These drugs are designed to be absorbed through your gut, travel through your bloodstream, and attack cancer cells from within. But because they’re processed by your liver and gut enzymes, tiny changes in how you take them can make a huge difference. There are four main types:- Alkylating agents like cyclophosphamide damage cancer cell DNA directly. They’re powerful but hit healthy cells too-causing nausea, hair loss, and low blood counts.
- Antimetabolites like capecitabine trick cancer cells into using fake building blocks, so they can’t copy their DNA. This often leads to hand-foot syndrome-red, peeling, painful skin on palms and soles.
- Topoisomerase inhibitors like topotecan stop cancer cells from untangling their DNA during division. They can cause severe diarrhea and low white blood cells.
- Mitotic inhibitors like vinca alkaloids freeze the cell’s internal scaffolding. These often cause nerve pain, numbness, or tingling in hands and feet.
The Hidden Dangers: Safety Risks You Can’t Ignore
You don’t need a nurse to give you this chemo. But that also means no one is watching you take it. And that’s where things go wrong. Drug interactions are the #1 safety issue. If you take an antacid, proton pump inhibitor (like omeprazole), or even St. John’s Wort with certain oral chemo drugs, your body might absorb only half the dose. For example, capecitabine’s effectiveness drops by 30-50% if you take it with antacids. The fix? Wait two hours before or after. Even common antibiotics or antifungals can be dangerous. Ketoconazole can spike your dasatinib levels by 325%, increasing the risk of internal bleeding. Rifampin can crash your lapatinib levels by 80%, letting cancer grow unchecked. Your pharmacist needs to know every pill, supplement, and herb you take-not just your oncologist. Storage and disposal matter too. Most oral chemo drugs need to be kept at room temperature (20-25°C). Don’t leave them in a hot car or a steamy bathroom. Some require refrigeration. Check the label. And never flush them down the toilet. Use FDA-approved disposal bags-available through your pharmacy or cancer center-to prevent environmental contamination and accidental exposure to pets or children.
Side Effects: What to Expect and When to Call
Side effects aren’t the same for everyone. But some are common enough to plan for:- Myelosuppression (low blood counts): This is the most serious. Your white blood cells drop, making you vulnerable to infection. Platelets fall, raising bleeding risk. Hemoglobin drops, causing fatigue. If you’re on dasatinib or lenalidomide, you’ll need weekly blood tests for the first month.
- Hand-foot syndrome: Starts as tingling or redness on palms and soles. Can progress to blisters, peeling skin, and pain so severe you can’t walk. Catch it early-cool your hands/feet, avoid tight shoes, and tell your team.
- Diarrhea and mucositis: Capecitabine and 5-FU analogs often cause loose stools or mouth sores. Don’t wait until it’s unbearable. Start anti-diarrheal meds early. Use saltwater rinses for mouth sores. Hydration is non-negotiable.
- Liver toxicity: 15-25% of patients show elevated liver enzymes. It’s often silent. That’s why blood tests every 2-4 weeks are mandatory.
- High blood pressure: Common with VEGF inhibitors like sunitinib. Check your BP at home. If it’s over 140/90, call your doctor.
- Skin rashes: EGFR inhibitors cause acne-like breakouts on the face and chest. They’re not just cosmetic-they can signal the drug is working. But if it’s painful or infected, treat it.
Adherence: The Silent Killer
Here’s the most shocking stat: only 55-75% of patients take their oral chemo exactly as prescribed. That means 1 in 3 people are getting less than full treatment. And that’s not because they’re careless. It’s because the system is broken. Complex schedules make it hard. Capecitabine? Twice a day for 14 days, then 7 days off. Nilotinib? Must be taken on an empty stomach-no food for 2 hours before or after. One missed dose can throw off the whole cycle. Studies show patients who get structured support have 82% adherence. Those who don’t? Only 58%. What’s the difference? Six things:- Initial education: At least 45 minutes with a trained nurse or pharmacist-not just a pamphlet.
- Teach-back method: “Tell me in your own words how you’ll take this.” If you can’t explain it, they haven’t taught it right.
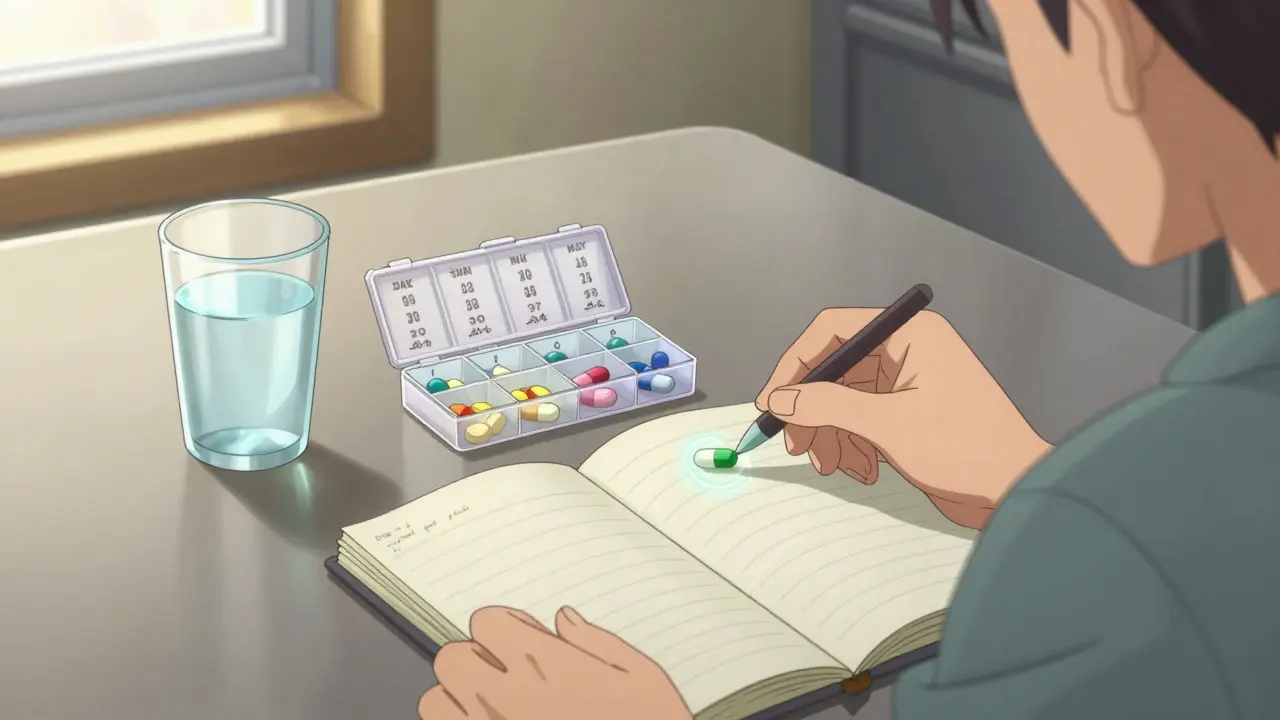
- Pill organizers: Not just any box. One with labeled compartments for each dose, day, and cycle.
- Follow-up calls: On day 3, day 7, day 14. Not just “How are you?” But “Did you have diarrhea? Did you take your pill with food?”
- Pharmacy refill tracking: If you don’t refill on time, they call you. Not to scold-to help.
- Rapid response: A direct line to someone who can adjust your meds or schedule an urgent appointment within 24 hours.

What’s Changing-And What’s Coming
The field is evolving fast. Fixed-dose combinations-like VerzenioPlus, which combines two drugs in one pill-are reducing pill burden. Ingestible sensors (like Proteus Discover) track when you swallow your dose and send alerts to your care team. Pharmacogenomic testing (like DPYD screening before capecitabine) cuts severe toxicity by 72%. Smart pill bottles with Bluetooth are in phase 3 trials. They don’t just remind you-they record if you opened the bottle, and if you took the pill. AI is being trained to predict who’s at risk of missing doses based on behavior patterns: missed appointments, delayed refills, or even changes in phone usage. But none of this replaces human connection. Technology helps. But if you’re scared, confused, or overwhelmed, you need someone to listen.What You Can Do Right Now
If you’re on oral chemotherapy:- Keep a written log: Date, time, dose, food intake, side effects.
- Use a pill organizer with separate compartments for each day and cycle.
- Never take a new medication-prescription, OTC, or supplement-without checking with your oncology pharmacist.
- Store your meds exactly as instructed. If you’re unsure, call your pharmacy.
- Know your emergency number. Don’t wait until Monday to call if you have a fever or can’t keep fluids down.
- Ask for a dedicated oncology pharmacist. They’re trained for this. Not every pharmacist is.
Can I split or crush my oral chemotherapy pill?
Never split, crush, or chew oral chemotherapy pills unless your oncologist or pharmacist specifically says it’s safe. Many are designed with special coatings to control how they’re absorbed. Crushing them can change how the drug works, increase toxicity, or expose you to dangerous dust. Always ask before altering your dose.
What should I do if I miss a dose?
Don’t double up. Call your oncology team immediately. Most oral chemo drugs have specific rules: if you miss a dose by less than 4-6 hours, you might take it right away. If it’s been longer, skip it and resume your regular schedule. Never guess. Your treatment plan is precise-missing a dose can affect your entire cycle.
Can I take oral chemotherapy with food?
It depends on the drug. Some, like capecitabine, work best with food. Others, like nilotinib or dasatinib, must be taken on an empty stomach-no food for 2 hours before and after. Always check the label or ask your pharmacist. Food can block absorption or spike blood levels, making the drug less effective or more toxic.
How do I know if my oral chemo is working?
You won’t feel it directly. Unlike IV chemo, where side effects sometimes signal activity, oral chemo works silently. Your team tracks progress through scans, blood tests, and tumor markers-not how you feel. Stick to your schedule, even if you feel fine. Skipping doses doesn’t make you feel better-it just lets cancer grow.
Is oral chemotherapy cheaper than IV chemo?
Not always. While you save on clinic visits, the drug itself is often more expensive. Many oral chemo drugs cost thousands per month and aren’t covered the same way as IV drugs under insurance. Some plans have higher copays for specialty oral meds. Always check your coverage and ask about patient assistance programs through the manufacturer.
Can I drink alcohol while on oral chemotherapy?
Most oncologists advise avoiding alcohol entirely. Alcohol can worsen liver toxicity, increase dehydration, and interfere with how your body processes chemo drugs. It can also make nausea, mouth sores, and fatigue worse. Even one drink a day may be too much. Ask your care team what’s safe for your specific regimen.

Bradford Beardall
January 11, 2026 AT 05:09I’ve been on oral chemo for 18 months and honestly, the biggest game-changer was getting an oncology pharmacist on my case. Not my regular pharmacy-this woman knew every drug interaction, every storage quirk, every damn pill schedule. She called me when my refill was late. She asked if I’d eaten before my nilotinib. She didn’t judge. She just showed up.
That’s the secret no one talks about: it’s not about willpower. It’s about having someone who treats your meds like a sacred ritual, not a chore.
McCarthy Halverson
January 12, 2026 AT 06:36Don’t crush the pills. Ever. Even if they’re big. Even if they taste awful. The coating’s there for a reason.
Michael Marchio
January 13, 2026 AT 15:49Let me tell you something about this whole oral chemo trend-it’s not about convenience, it’s about cost-cutting. Hospitals don’t want to pay for nurses, IV bags, clinic space. So they shove the burden onto patients who are already drowning in fear and fatigue. And then they act like it’s your fault when you miss a dose?
Meanwhile, the drug companies are making billions off these pills while insurance companies fight every copay. You think they care if your liver enzymes spike? No. They care if your deductible gets met.
And don’t even get me started on those ‘smart pill bottles.’ They’re not helping you. They’re monitoring you. Tracking your behavior. Selling your data to pharma. This isn’t innovation. It’s surveillance dressed up as care.
And don’t tell me about ‘patient support programs.’ Those are marketing gimmicks. The real support? A $2000 pill with a $1500 copay and a 3-week wait for a nurse to call back. That’s the system we’re celebrating.
They call it empowerment. I call it abandonment with a side of guilt.
Jake Kelly
January 15, 2026 AT 02:18I’m two months into capecitabine and I’ve been keeping a little notebook. Time, dose, food, side effects. It’s simple but it helps. I showed it to my oncologist last week and she actually smiled. Said it was the most detailed log she’d seen in months.
It’s not about being perfect. It’s about showing up. Even just a little.
Ashlee Montgomery
January 16, 2026 AT 20:23There’s a quiet dignity in taking your medicine at home. No one sees you swallow it. No one watches you wince. No one asks if you’re okay.
But that silence is heavy. It’s not freedom-it’s isolation wrapped in convenience.
I wish more people understood that adherence isn’t discipline. It’s love. Love for the person you were before diagnosis. Love for the future you still believe in.
And if you miss a dose? It doesn’t mean you failed. It means you’re human. Call your team. Don’t hide. You’re not alone in this silence.
neeraj maor
January 17, 2026 AT 10:39Oral chemo is a Trojan horse. The FDA and Big Pharma pushed this to avoid oversight. They know most patients can’t track interactions. They know people take it with grapefruit juice or ibuprofen. They know storage is ignored. And they know the liver enzyme data is messy.
Meanwhile, the real cancer killers are still IV-because they’re controlled, monitored, dosed by professionals. Oral chemo? It’s a profit model disguised as progress. Look at the patents. Look at the pricing. Look at the lawsuits.
And don’t tell me about ‘smart bottles.’ That’s just the next step in turning patients into data points for AI-driven insurance denials.
This isn’t medicine. It’s capitalism with a stethoscope.
Ritwik Bose
January 17, 2026 AT 15:03Thank you for sharing this comprehensive and deeply thoughtful overview 🙏
I am from India and have seen firsthand how access to proper oncology pharmacy support varies drastically-even within urban centers. The mention of FDA-approved disposal bags was especially meaningful; here, many patients simply throw pills in the trash or flush them, unaware of the environmental and familial risks.
I hope more healthcare systems adopt the six pillars of adherence you described. Education, follow-up, and human connection are not luxuries-they are lifelines.
May we all find strength in small, consistent acts of care.
With respect and hope 🌿
Paul Bear
January 18, 2026 AT 23:42Let’s be precise here: the 55-75% adherence rate isn’t a failure of patient discipline-it’s a systemic failure of pharmacokinetic education. Oral chemotherapeutics exhibit first-pass metabolism via CYP3A4 and UGT1A1, and their bioavailability is highly susceptible to P-glycoprotein modulation. When patients concomitantly ingest PPIs (e.g., omeprazole), they induce gastric pH shifts that alter dissolution kinetics of weakly basic compounds like dasatinib, reducing Cmax by up to 50% and AUC by 30%.
Moreover, the notion that ‘storing meds in the bathroom’ is merely negligent is an understatement-humidity levels above 60% RH can trigger hydrolytic degradation of capecitabine, yielding 5-fluorouracil precursors that increase toxicity risk.
And for the record: alcohol isn’t just ‘advised against.’ Ethanol competitively inhibits alcohol dehydrogenase, which metabolizes 5-FU’s intermediate metabolites, leading to prolonged half-life and cumulative myelosuppression. This isn’t opinion-it’s clinical pharmacology.
Bottom line: if your care team isn’t discussing CYP isoforms and bioavailability curves, you’re not getting optimal care. Ask for a clinical pharmacist. Demand it.