You switch from your brand-name pill to the generic version because it’s cheaper. A few days later, you start feeling dizzy, your muscles ache, and you feel unusually tired. You blame the new medication. But here’s the twist: you didn’t actually switch medications. You switched packaging. The active ingredient is identical. So why do you feel worse?
This isn’t rare. It’s called the nocebo effect-when negative expectations about a treatment trigger real physical symptoms, even when the treatment is harmless. With generic medications, this isn’t just a psychological quirk. It’s a widespread, costly, and often misunderstood problem that’s undermining patient health.
What Exactly Is the Nocebo Effect?
The word "nocebo" comes from Latin, meaning "I shall harm." It’s the dark twin of the placebo effect. Where placebo makes you feel better because you believe a treatment works, nocebo makes you feel worse because you believe it won’t-or will hurt you.
Studies show that when patients are told a pill might cause side effects, even if it’s just a sugar pill, they report those side effects at alarming rates. In clinical trials, about 1 in 5 people taking a placebo report headaches, nausea, or fatigue. Nearly 1 in 10 quit the trial altogether-because they thought the medicine was making them sick.
It’s not in their heads. Brain scans show that negative expectations light up the same areas that process pain and anxiety. When someone is told an injection will feel like a "bee sting," they report more pain than someone told it will be "comfortable." The body reacts to belief as if it’s real.
Why Generics Trigger the Nocebo Effect
Generic drugs are chemically identical to brand-name versions. They contain the same active ingredient, in the same dose, and must pass strict bioequivalence tests to be approved. But patients don’t always know that.
When a pharmacist swaps your brand-name statin for a generic, the pill looks different. The label says "generic." The price is lower. And if you’ve heard stories-"My cousin switched and got awful muscle pain," or "Generics don’t work as well"-your brain starts scanning for trouble.
Normal body sensations become proof of harm. A little fatigue? Must be the new pill. A mild headache? Must be the generic. A stomach upset? Definitely the switch. Even if you’ve never had these symptoms before.
One study found patients told that beta-blockers could cause sexual side effects were 3 to 4 times more likely to report them-despite taking the exact same drug as the control group. Another found that 45% of people who reported muscle pain after switching to generic statins still felt it-even after going back to the brand-name version.
The problem isn’t the drug. It’s the story.
How Doctors and Pharmacies Make It Worse
It’s not just patients. Sometimes, the people giving the medication are the ones planting the seed of doubt.
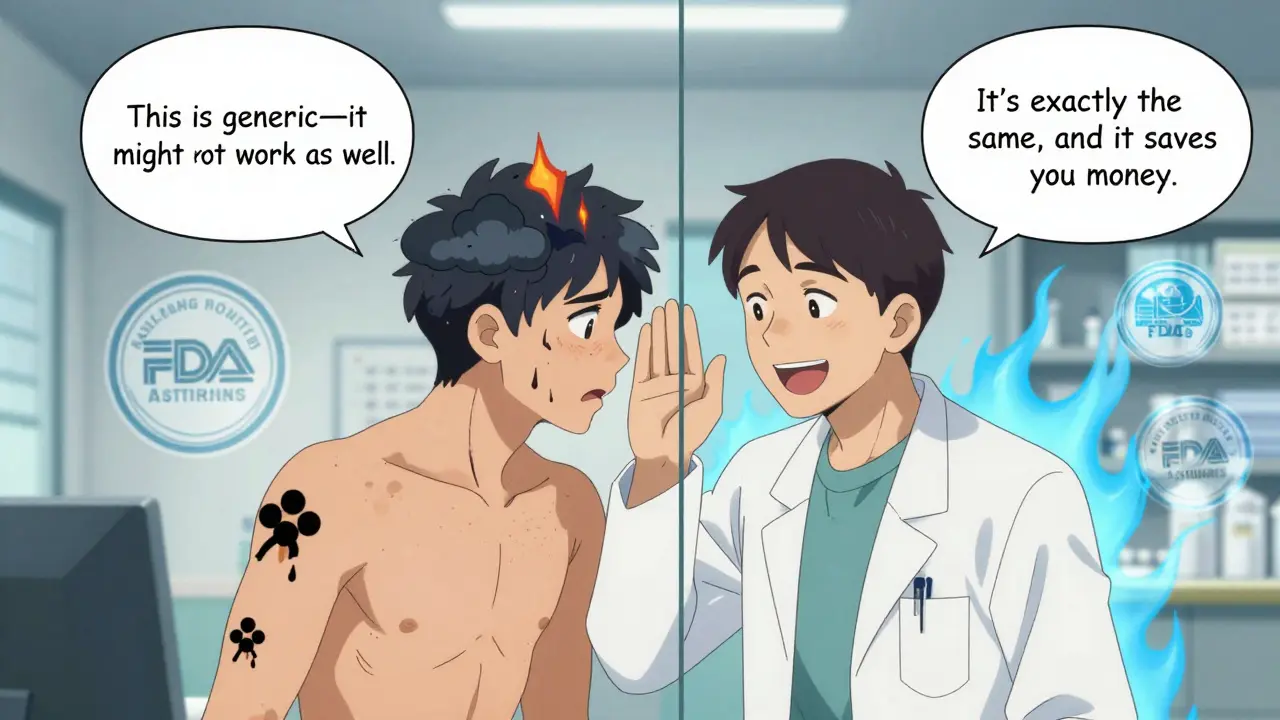
Doctors who say things like, "This is the generic version-it’s cheaper, but might not work as well," or pharmacists who hand over a new pill with a sigh and say, "It’s the same, but you might notice a difference," are accidentally triggering the nocebo effect.
Research shows that when patients are told a generic might be "less effective," they report 65% more side effects than those told it’s "just as good." On the flip side, when clinicians say, "This works exactly like your old pill and will save you money," patient-reported side effects drop by 37%.
Even the way information is written on the packaging matters. A 2022 FDA guidance now requires generic drug leaflets to avoid language that implies inferiority. Phrases like "may cause more side effects" or "different formulation" are being replaced with "same active ingredient" and "clinically equivalent."
Real Cases: When Belief Overrules Biology
In New Zealand in 2017, a major switch from brand-name venlafaxine to its generic version caused a spike in adverse effect reports. But here’s the catch: when the medication was first switched, reports stayed normal. It wasn’t until news outlets ran stories warning about "problems with the generic" that reports exploded. The drug hadn’t changed. The fear had.
Another study looked at patients switched from brand-name to generic antidepressants. Those who received no explanation about the switch had a 12% rate of new side effects. Those who were told, "This is a generic, and some people report changes," had a 32% rate.
Reddit threads are full of stories like this: "Switched to generic lisinopril, got a rash. Went back to brand-rash vanished." But when tested in controlled settings, the rash was never linked to the drug. It was linked to the belief that the generic was "different."
The Economic and Health Cost of Nocebo
This isn’t just about feeling bad. It’s about real harm.
When patients stop taking their medication because they think the generic isn’t working, their condition worsens. Blood pressure rises. Cholesterol climbs. Depression returns. They end up back in the doctor’s office-with a brand-name prescription, higher costs, and more risk.
Research published in JAMA Internal Medicine estimates that nocebo-driven discontinuation of generic medications costs the U.S. healthcare system $1.2 billion a year. That’s billions spent on unnecessary brand-name drugs, extra doctor visits, and emergency care-all because of a belief, not a chemical.
The World Health Organization lists negative perceptions about generics as a key barrier to medication adherence in 67% of countries. And in the U.S., where 90% of prescriptions are filled with generics, that’s millions of people at risk of harm-not from the drug, but from their own expectations.
How to Fight the Nocebo Effect
There’s good news: the nocebo effect can be reduced-and even reversed-with the right communication.
Here’s what works:
- Don’t mention the word "generic" unless necessary. Instead, say: "This is the same medicine you were taking, just a different brand."
- Emphasize equivalence. "The FDA requires generics to work exactly like the brand-name version. They’re tested to be just as safe and effective."
- Reframe expectations positively. "This will help you save money without losing any benefit. Many people switch without any issues."
- Normalize normal sensations. "It’s common to notice small changes in how you feel when you start a new pill-even if it’s the same drug. That doesn’t mean it’s not working."
- Train providers. Doctors and pharmacists who get training on the nocebo effect reduce patient-reported side effects by 28%.
Some clinics are even using AI tools that tailor messages based on a patient’s past beliefs and anxiety levels. Early results show a 41% drop in nocebo responses.
What You Can Do Right Now
If you’re about to switch to a generic:
- Ask your pharmacist: "Is this the same medicine as my old one?"
- Don’t Google side effects before you start. That’s like reading horror stories before bed-you’ll start feeling the symptoms before they happen.
- If you feel weird after switching, wait a week. Don’t assume it’s the pill. It could be stress, sleep, or just your body adjusting.
- If symptoms persist, talk to your doctor. But don’t automatically go back to the brand. Ask: "Could this be the nocebo effect?"
If you’re a caregiver or someone helping a loved one switch:
- Don’t say, "I hope this works better than the last one." That plants doubt.
- Instead, say: "This is the same medicine. It’s just cheaper. You’re still getting the same treatment."
The Bigger Picture
Generic medications save lives. They make treatment possible for people who couldn’t afford it before. But if we keep treating them like second-class drugs, we’ll keep making people sick-not because of the medicine, but because of what we tell them about it.
The science is clear: your belief changes your biology. And when it comes to generics, the most powerful drug isn’t the pill in your hand-it’s the story you’ve been told about it.
It’s time to stop telling the wrong story.

