Imagine taking a pill every day because the label says ‘once daily’-but you don’t know what that means. You’ve never heard the phrase before. The only person who could explain it is your grandchild, who’s in school. You’re scared to ask. So you take it twice a day, just to be safe. That’s not a rare mistake. It’s happening right now in pharmacies across Australia, the U.S., Canada, and beyond. For millions of non-English speakers, medication instructions aren’t just hard to read-they’re dangerous.
Why Medication Labels Can Be Deadly
Prescription labels aren’t written for patients. They’re written for pharmacists. Terms like ‘QD,’ ‘BID,’ ‘PRN,’ or ‘take with food’ mean nothing to someone who doesn’t speak English. Even simple words like ‘daily’ can be misread. One Korean patient in a 2023 study took her blood thinner twice a day because she thought ‘daily’ meant ‘every day’-not ‘once per day.’ That’s the kind of mistake that leads to strokes, hospital visits, or worse. Studies show non-English speakers are 1.5 to 3 times more likely to have a serious medication error. In one 2020 survey, 78% of non-English speaking patients said they didn’t understand their instructions. For Vietnamese speakers, that number jumped to 87%. And it’s not just about language-it’s about culture. Some patients avoid taking medicine because they think side effects are ‘bad luck’ or ‘punishment.’ Others skip doses because they believe the pill is too strong. Without clear, culturally aware explanations, safety becomes a lottery.What Works: The Right Way to Translate Medication Instructions
Not all translations are created equal. A machine translation from Google Translate? Risky. A bilingual pharmacy tech who learned a few phrases? Not enough. The only proven method is professionally translated, medically validated instructions. Projects like ConcordantRx tested simple, plain-language labels in Chinese, Korean, and Russian. Instead of saying ‘take one tablet by mouth twice daily,’ they wrote: ‘Take one pill in the morning and one pill at night.’ No medical jargon. No abbreviations. Just clear, everyday words. The result? 100% of patients understood their instructions. Compare that to traditional translations-only 45% understood. Good labels also use pictures. A pill with a clock next to it means ‘take at the same time every day.’ A red stop sign means ‘don’t drink alcohol.’ These symbols follow ISO 3864 and FDA guidelines. They work even if you can’t read a single word.How Pharmacies Are (and Aren’t) Helping
In Australia, Canada, and the U.S., laws say pharmacies must provide language access. But laws don’t mean action. Only 57% of community pharmacies offer translated labels, according to a 2021 survey. In hospitals, it’s better-78% do. But small, independent pharmacies? Only 32%. Why? Cost. Professional translation adds $2.50 to $5.00 per prescription. Many pharmacies say they can’t afford it. But the real cost is higher. Medication errors lead to emergency visits, hospital stays, and lawsuits. A 2023 study found pharmacies with good language services had 15% lower costs from medication-related hospitalizations. Some pharmacies try to cut corners. They use family members as interpreters. Bad idea. A 2022 report found this leads to 65% more errors. Kids translating for parents? Too risky. Even trained bilingual staff only get 42% comprehension rates. That’s worse than flipping a coin.
The Best System: Three Layers of Safety
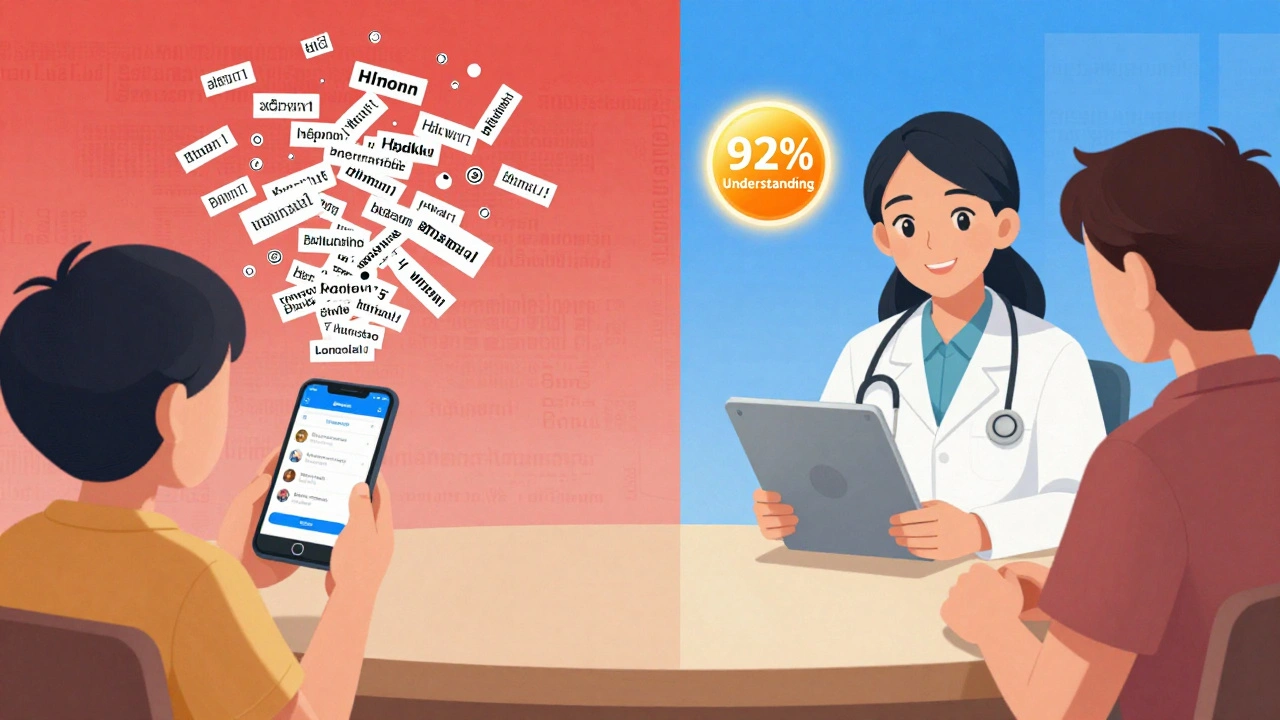
The most effective approach isn’t just one thing-it’s three things working together:- Bilingual labels with plain language and pictograms. These are the first line of defense.
- Professional interpreter services during counseling. A trained medical interpreter doesn’t just translate words-they explain meaning. This gets 92% understanding rates.
- Culturally tailored education. A handout showing how to store insulin in a hot climate, or explaining why a heart pill can’t be stopped suddenly-these matter. One study showed 85% of patients retained info better when it matched their cultural beliefs.
What You Can Do: A Patient’s Guide
If you or someone you care about doesn’t speak English well, here’s how to protect yourself:- Ask for your preferred language when you drop off the prescription. Say: ‘Can you print this label in [language]?’ Don’t wait until you get home.
- Request a face-to-face talk with a certified medical interpreter. Don’t accept a staff member who just ‘knows a little Spanish.’ Ask if they’re certified.
- Check the label for pictures. If there are none, ask if they have a version with symbols.
- Bring a trusted friend or community health worker to the pharmacy. They can help ask questions.
- If you’re confused, call the pharmacy back. Say: ‘I didn’t understand the instructions. Can you explain them again in [language]?’
The Future Is Changing-Slowly
Change is coming. California now requires all pharmacies to be certified in language access as of January 2024. New York City mandates translations for the top 10 languages. The federal government is pushing for EHR systems to automatically flag language needs and trigger translations. AI translation tools are being tested, but the FDA warned in 2023: unvalidated AI tools make 43% of medication instructions wrong. That’s not progress-it’s a danger. The real solution? More trained medical translators. Right now, there are only 12 certified translators for Hmong and Navajo in the entire U.S. We need more. We need better training. We need pharmacies to treat language access like a safety system-not an optional add-on.It’s Not Just About Words-It’s About Trust
Medication safety isn’t just about reading a label. It’s about trust. When a patient doesn’t understand their medicine, they stop trusting the system. They stop asking questions. They hide their confusion. That’s when accidents happen. Clear instructions don’t just prevent errors. They restore dignity. They let people take control of their health. A simple translated label says: ‘We see you. We care. You belong here.’ The technology exists. The research proves it works. The laws require it. What’s missing is the will to do it right.Can I ask my pharmacy to translate my prescription label?
Yes, you have the legal right to ask. Under civil rights laws, pharmacies must provide meaningful access to information in your preferred language. Ask when you drop off your prescription. If they say no, ask to speak to the manager or file a complaint with your state pharmacy board.
Are free translation apps safe for reading medicine labels?
No. Apps like Google Translate or DeepL often mistranslate medical terms. One study found automated tools made errors in 38% of medication instructions. Words like ‘intravenous’ or ‘sublingual’ get turned into nonsense. Even simple phrases like ‘take with food’ can be misinterpreted. Always rely on professionally translated labels or a certified interpreter.
What if my language isn’t supported by the pharmacy?
If your language isn’t available, ask if they can connect you with a phone or video interpreter. Many pharmacies use services like LanguageLine or RxTran that offer 25+ languages, including less common ones like Somali, Tagalog, or Farsi. If they can’t help, contact a local community health center-they often have translators on staff or can refer you to one.
Why don’t more pharmacies offer translated labels?
Cost and lack of awareness. Professional translation adds $2.50-$5.00 per prescription, and many small pharmacies think they can’t afford it. But the real cost is higher: medication errors lead to hospital visits, lawsuits, and lost trust. Some pharmacies also don’t know how to set up the system or think it’s optional. It’s not. Federal law requires it.
How do I know if a translator is qualified?
Ask if they’re certified by a national medical interpreting board, like the National Board of Certification for Medical Interpreters (NBCMI) or CCHI. Certified interpreters have passed exams in medical terminology, ethics, and confidentiality. Don’t accept someone who says they ‘grew up speaking Spanish’ or ‘learned it in high school.’ Medical terms are too dangerous to guess.


Jennifer Blandford
December 11, 2025 AT 07:10My abuela took her blood pressure med twice a day for three months because she thought 'daily' meant 'every day'-not 'once.' She almost ended up in the ER. This post? It’s not just important-it’s life-saving. I’m sharing this with every family group chat I’m in.
Brianna Black
December 12, 2025 AT 02:20Let me tell you about the time my cousin’s mom got her insulin label in Tagalog… and it said 'inject in the arm' instead of 'thigh.' The translator used Google Translate. She nearly went into diabetic shock. 🤯 This isn’t a language issue-it’s a systemic failure. We need certified interpreters in every pharmacy, period. No excuses.
Ronald Ezamaru
December 12, 2025 AT 20:22As a pharmacist in rural Ohio, I’ve seen this firsthand. We started using pictogram labels with plain language translations last year. Compliance jumped from 52% to 89% among non-English speakers. The cost? $3.50 per script. The savings? Over $120K in avoided ER visits last year alone. It’s not charity-it’s smart business. And it’s the bare minimum we owe our patients.
Asset Finance Komrade
December 14, 2025 AT 03:49Interesting. But isn’t this just another case of society infantilizing non-English speakers? Why not teach them English? We all had to learn the language of the country we live in. If you can’t read the label, maybe you shouldn’t be taking the pill. It’s not the pharmacy’s job to be a global translator service. 🤷♂️
Ryan Brady
December 16, 2025 AT 00:12Yeah right. Next you’ll want the FDA to print labels in Klingon. We’ve got 50 million immigrants here. Do you know how much that costs? We’re already drowning in regulations. Let them learn English or go back to their country. This is America. 🇺🇸
Raja Herbal
December 16, 2025 AT 00:30So let me get this straight… we spend millions on AI that mistranslates 'sublingual' as 'under the tongue'… but we won’t pay $5 to hire a real translator? 🤦♂️ In India, we have 22 official languages and still manage to get pills right. Guess what? We don’t rely on kids or Google. We train people. Just saying.
Shubham Mathur
December 17, 2025 AT 12:46My sister works in a pharmacy in Chicago. She told me they tried using family members for interpretation once. A 12-year-old told his grandfather his heart med was 'for headaches.' Grandpa took it every time he got a migraine. For six months. He ended up with internal bleeding. No one laughed. No one joked. We lost a good man because we thought 'they’ll figure it out.' This isn’t about language. It’s about dignity. And if you think $5 is too much to pay for that… you’ve never held someone’s hand while they’re scared to ask if the pill will kill them.
Stacy Tolbert
December 18, 2025 AT 19:25My mom’s 78. She’s been taking warfarin for 12 years. She still doesn’t know what 'QD' means. I cry every time I have to explain it again. This system is broken. But the worst part? She’s too ashamed to ask. She thinks she’s dumb. We need to fix this-not just for her, but for every grandparent who’s too proud to say 'I don’t understand.'