When someone is managing a mental health condition, medication isn’t just another pill in a routine-it’s often the difference between stability and crisis. But here’s the hard truth: medication safety in mental health care is falling through the cracks. People are getting the wrong dose, missing critical blood tests, or having their meds stopped abruptly during hospital transfers-all because systems aren’t talking to each other. And the consequences? Hospitalizations, overdoses, even deaths that could have been prevented.
Why Mental Health Medications Are Different
Psychotropic drugs aren’t like antibiotics or blood pressure pills. They affect how your brain works. Lithium, clozapine, valproate-these aren’t just medications. They’re high-alert drugs. One wrong dose, and you could end up with kidney damage, seizures, or life-threatening blood disorders. Yet, they’re often prescribed in settings where staff aren’t trained to handle them safely. In general medical wards, nurses check the five rights: right patient, right drug, right dose, right route, right time. In mental health units? Many still rely on paper charts, unclear handwriting, and rushed handovers. A 2021 review from New Zealand’s Health Quality & Safety Commission found that over 40% of medication errors in psychiatric care happened during transitions-when someone moved from a hospital to a community clinic, or from prison to home. And it’s not just about mistakes. Patients with serious mental illness often struggle with memory, motivation, or trust. They might skip doses because they don’t feel like taking pills. Or they might hide them to sell or trade. One nurse in Saskatchewan told me, “I’ve had patients swallow meds and then say they didn’t take them. We have to watch them take every pill-no exceptions.”The Breakdown in Care Coordination
Imagine this: You’re discharged from a psychiatric hospital on lithium. Your discharge summary says “continue 600mg daily.” But your GP, who’s never treated someone on lithium before, doesn’t know you need monthly blood tests to check your kidney and thyroid function. Three months later, you’re dizzy, nauseous, and your lithium level is dangerously high. That’s not a rare case. In England, only 40% of patients on lithium get the required blood tests in primary care. Why? Because mental health care and physical health care are still treated like separate worlds. Your psychiatrist sees you every six weeks. Your GP sees you for a cold. Your pharmacist fills the script. Nobody connects the dots. NHS England’s 2017 guidelines pointed this out clearly: “Medicines reconciliation must happen every time a person moves between settings.” But in practice? It rarely does. In prisons, where mental illness rates are 3-5 times higher than the general population, medication errors are even more common. People come in on one set of meds, get switched without proper review, and leave with no plan.What Actually Works: The Proven Fixes
The good news? We know what reduces harm. And it’s not fancy tech-it’s simple, repeatable systems.- Medicines reconciliation isn’t optional. Every time someone enters or leaves a hospital, prison, or care home, their entire medication list must be reviewed side-by-side with what they were taking before. No assumptions. No “I think they were on…”
- Electronic prescribing cuts prescribing errors by up to 55%. No more illegible handwriting. No more wrong doses because someone misread “0.5” as “5.”
- Clinical pharmacists embedded in mental health teams reduce errors by 25%. They spot drug interactions, check if a dose is too high for an elderly patient, or flag that mirtazapine is being used off-label for sleep-something NHS England warns can lead to abuse.
- The ten rights and three checks (used in Saskatchewan and adopted elsewhere) go beyond the basics. Right patient. Right medication. Right dose. Right route. Right time. Right documentation. Right reason. Right response. Right to refuse. Right education. And you check all of them before, during, and after giving the med.
Polypharmacy: The Silent Killer
Many people on mental health meds are also taking pills for diabetes, high blood pressure, pain, or sleep. That’s not unusual. But when you stack five, six, or seven drugs together-especially with antipsychotics, antidepressants, and benzodiazepines-the risk of dangerous interactions skyrockets. A 2023 study in the UK found that 1 in 3 patients on multiple psychotropics had at least one potentially harmful interaction. Some combinations can slow your heart to a dangerous rhythm. Others can make you fall over from dizziness. Yet, prescribers rarely sit down and ask: “Do you really need all of these?” NICE guidelines say: “Ask three questions before prescribing: Is it safe? Does it work? Is it necessary?” Too often, the answer is “We’ve always done it this way.” The fix? Regular med reviews. Every three months. With the patient present. With a pharmacist. With a checklist. If a drug isn’t helping, or if it’s causing more harm than good, it should come off. Not just “left on” because no one remembered to take it off.Who’s Responsible? The Culture Shift
Medication safety isn’t just the job of the psychiatrist or the pharmacist. It’s everyone’s job. - Doctors need to write clear, specific prescriptions-not “take as needed” for antipsychotics. Include the reason: “For auditory hallucinations, not sedation.” - Nurses need training on high-alert meds. Not just how to give them, but how to spot early signs of toxicity. - Pharmacists need access to mental health records. Right now, most community pharmacies don’t even know their patient is on clozapine. - Patients need to be partners, not passive recipients. They should know why each med is prescribed, what side effects to watch for, and who to call if something feels wrong. And here’s the biggest barrier: blame culture. When something goes wrong, people get punished. That makes staff hide mistakes. The fix? A “just culture.” One where errors are reported without fear, systems are fixed, and learning happens. The American Society of Health-System Pharmacists says this isn’t optional-it’s foundational.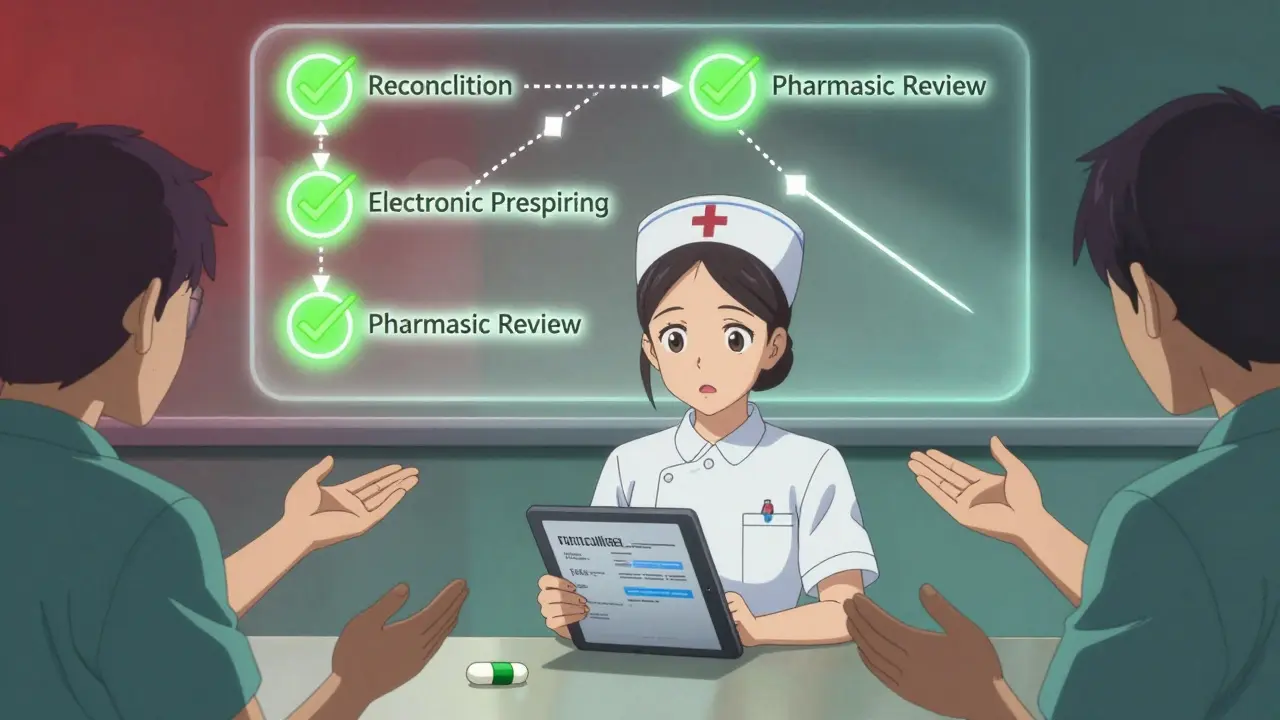
What You Can Do Right Now
If you’re a patient or a caregiver:- Keep a written list of every medication you take-including doses, times, and why you’re taking them.
- Ask your prescriber: “Is this still necessary? Could anything be taken off?”
- For lithium, clozapine, or valproate: Ask if you need regular blood tests-and if you’ve had them in the last 3 months.
- Don’t stop meds suddenly. Even if you feel fine, some drugs can cause seizures or psychosis if stopped cold turkey.
- Ask for a care coordinator. Someone who knows your whole history and can make sure your GP, psychiatrist, and pharmacist are all on the same page.
- Use electronic prescribing. If your clinic still uses paper, push for change.
- Start every visit with: “What meds are you taking now?” Not “Are you still on your meds?”
- Document the reason for every prescription. Not just “depression.” Say “sertraline for low mood and fatigue, target dose 100mg.”
- Involve a pharmacist in your team meetings. Even once a month.
The Bottom Line
Medication safety in mental health isn’t about perfection. It’s about reducing preventable harm. We know how to do it. We’ve got the tools. We’ve got the guidelines. What’s missing is the will to make it routine. The WHO calls mental health medication safety a “high-risk situation” for a reason. But high-risk doesn’t mean hopeless. It means urgent. And urgent means acting now-before the next person falls through the cracks.What are the most dangerous mental health medications?
Lithium, clozapine, and valproate are classified as high-alert medications because they have narrow therapeutic windows. Lithium can cause kidney or thyroid damage if blood levels aren’t monitored. Clozapine can drop white blood cell counts to dangerous levels, requiring weekly blood tests. Valproate can cause liver toxicity and birth defects. These aren’t “bad” drugs-they’re powerful ones that need strict oversight.
Why do mental health patients have more medication errors?
Patients with serious mental illness often face cognitive challenges, communication barriers, or lack of insight into their condition. They may not remember to take meds, may hide them, or may not understand why they’re prescribed. Add to that fragmented care between hospitals, GPs, and community services, and the system becomes full of gaps. Unlike general medical care, mental health settings rarely have standardized safety checks built in.
Can a GP safely manage mental health medications?
Yes-but only if they’re supported. Many GPs aren’t trained in psychopharmacology. A 2023 NIH study found that lack of mental health knowledge among general practitioners is a major contributor to prescribing errors. The solution isn’t to keep all mental health meds with psychiatrists-it’s to give GPs better training, access to specialists, and tools like shared care plans and clinical pharmacist support.
What’s medicines reconciliation, and why does it matter?
Medicines reconciliation is the process of comparing a patient’s current medication list with what they were taking before a care transition-like going from hospital to home. It catches errors like missed meds, duplicate prescriptions, or wrong doses. New Zealand’s health commission found this single step reduces medication discrepancies by up to 70%. Skipping it is like driving blindfolded.
How can I tell if my loved one’s meds are being managed safely?
Ask: Do they have a written list of all their meds? Are they getting regular blood tests (especially for lithium or clozapine)? Has anyone reviewed all their meds in the last 3 months? Are they seeing the same pharmacist or care coordinator regularly? If the answer to any of these is no, it’s time to speak up. Safety isn’t automatic-it’s built by asking questions.


Samar Khan
December 28, 2025 AT 18:31OMG this is SO real 😭 I had a cousin on lithium and no one checked her levels for 8 months… she ended up in the ER with tremors and kidney pain. Her GP just assumed the psychiatrist handled it. Why do we treat mental health like it’s not PHYSICAL? 🤦♀️
Nicole K.
December 30, 2025 AT 04:44This is why people shouldn’t be allowed to take psychiatric meds without a guardian. If you can’t even remember to take your pills, how can you be trusted with life-altering drugs? It’s irresponsible.
Fabian Riewe
December 30, 2025 AT 19:11Love this breakdown. Seriously. I’m a nurse in a psych unit and we’ve started using the 10 rights + 3 checks since last year. It’s a little slower at first, but the number of near-misses dropped by like 70%. People think it’s overkill, but when you’ve seen someone go into toxic psychosis from a simple dosing error? You don’t skimp. 💪
Amy Cannon
December 30, 2025 AT 20:14It’s absolutely unforgivable that we still allow paper charts in psychiatric care in 2024. I mean, come on. We have smartphones that can track our poop, but we can’t digitize medication lists for people who might die if they miss a blood test? This isn’t just negligence-it’s systemic ableism wrapped in bureaucracy. 🤦♀️
Himanshu Singh
December 31, 2025 AT 20:16Great post! I work in a clinic in Delhi and we just started using shared digital care plans with our psychiatrists and GPs. Took 6 months to get everyone on board, but now our lithium check rate went from 30% to 85%. Small steps, but it works! 😊
Sharleen Luciano
January 2, 2026 AT 13:14Let’s be honest-most GPs shouldn’t be prescribing antipsychotics. They don’t understand pharmacokinetics, they don’t know the difference between clozapine and quetiapine, and they’re too busy chasing KPIs to care. This isn’t a system failure-it’s a credentialing failure.
Emma Duquemin
January 3, 2026 AT 18:11Y’ALL. I’m a peer support specialist and I’ve seen people get discharged with 7 meds and no one telling them what half of them do. One guy thought his antihistamine was for anxiety. Another stopped her valproate because she read online it causes hair loss-so she had a seizure. We need to treat meds like they’re dynamite. Because they are. 🔥
Kevin Lopez
January 5, 2026 AT 14:43Polypharmacy risk stratification is non-negotiable. QTc prolongation + CYP450 interactions + CNS depression = perfect storm. Stop prescribing benzodiazepines as sleep aids. Period.
Duncan Careless
January 6, 2026 AT 16:43Just wanted to say I’ve seen this in the UK too. My mum was on clozapine and her GP didn’t know she was even on it until I showed them the script. Took three calls to the pharmacy to get them to check the NHS record. It’s not just broken-it’s invisible.
Russell Thomas
January 7, 2026 AT 23:35Oh wow, so now we’re blaming the patients for not remembering their meds? Cool. Let’s also blame the homeless guy for not having a fridge to store his insulin. Real empathetic.
Joe Kwon
January 8, 2026 AT 02:24Agreed with Fabian. We use the 10 rights in our unit and it’s saved lives. Also, having a pharmacist come in once a week to review med lists? Game changer. No more "we’ve always done it this way." 🙌
Jasmine Yule
January 8, 2026 AT 20:30I’m a mom of a teen on antipsychotics. I keep a color-coded spreadsheet with every med, dose, blood test date, and side effect. I print it and hand it to every new doctor. If you’re not doing this, you’re gambling with their life. I’m not being dramatic-I’m being a parent.
Greg Quinn
January 10, 2026 AT 05:57It’s interesting how we treat medication safety like a technical problem, when it’s really a human one. We build systems to fix errors, but we don’t fix the isolation, the stigma, the exhaustion that makes people forget pills or hide them. Maybe the real fix isn’t more checks-it’s more connection.
Lisa Dore
January 11, 2026 AT 18:26Thank you for writing this. I’m a peer advocate and I run a free medication safety workshop every month. We teach people how to make their own med list, how to ask for blood tests, and how to say "I need a review" without feeling guilty. It’s not glamorous, but it saves lives. Let’s keep talking.