Macrolide Heart Risk Calculator
Risk Assessment
This tool helps determine your risk of developing QT prolongation when taking macrolide antibiotics like azithromycin or clarithromycin. Based on the latest clinical guidelines, this assessment will help you and your doctor make safer prescribing decisions.
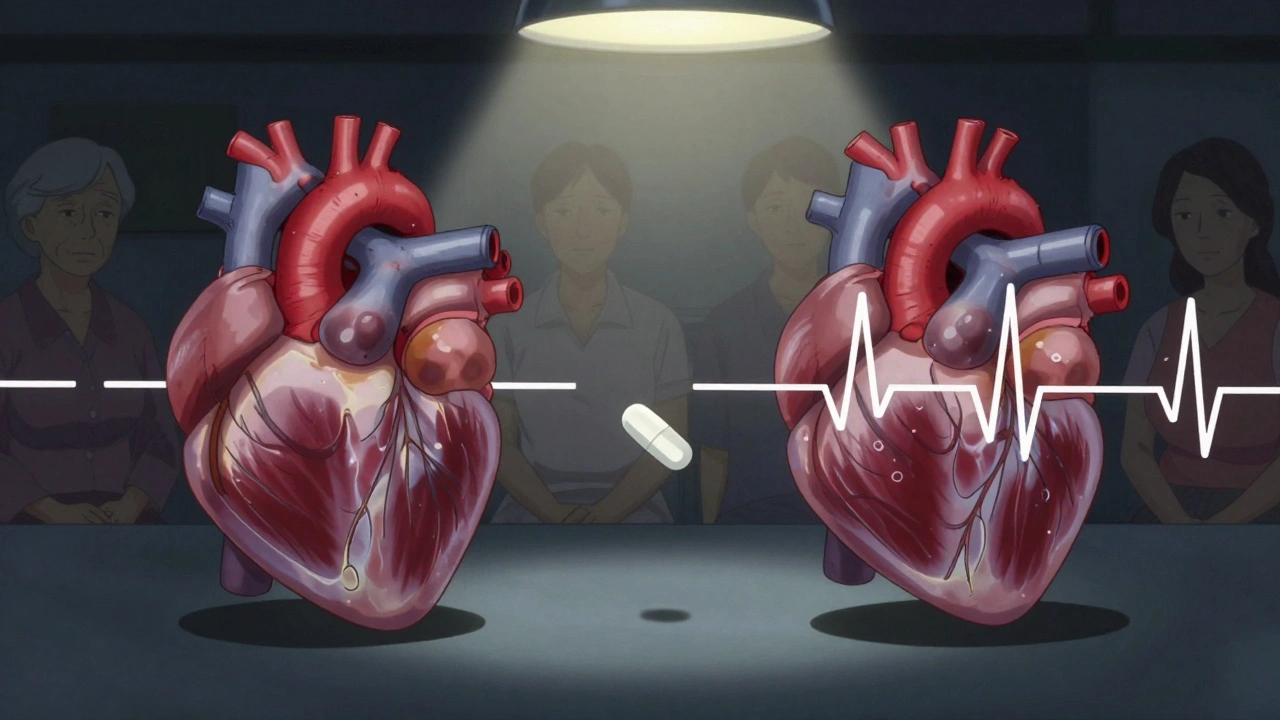
When you take a macrolide antibiotic like azithromycin or clarithromycin for a sinus infection or bronchitis, you’re probably thinking about getting better-not about your heart. But for some people, these common drugs can trigger a dangerous heart rhythm problem called QT prolongation, which can lead to a life-threatening arrhythmia known as Torsades de pointes. This isn’t theoretical. It’s real, documented, and preventable-if you know the signs and risks.
What Are Macrolide Antibiotics?
Macrolide antibiotics include azithromycin, clarithromycin, and erythromycin. They’ve been around since the 1950s and are widely used for respiratory infections, skin infections, and some sexually transmitted diseases. Azithromycin is especially popular because it’s often given as a single 500 mg dose followed by four 250 mg doses-convenient for patients and doctors alike. But convenience doesn’t mean safety for everyone.
These drugs work by stopping bacteria from making proteins they need to survive. But they also interact with your heart’s electrical system. Specifically, they block a potassium channel called Ikr, which is encoded by the hERG gene. This channel helps your heart reset after each beat. When it’s blocked, the heart takes longer to repolarize, and that delay shows up on an ECG as a longer QT interval.
Why QT Prolongation Matters
The QT interval measures how long it takes your heart’s ventricles to recharge between beats. A normal QTc (corrected for heart rate) is under 450 ms in men and under 470 ms in women. When it stretches beyond 500 ms-or increases by more than 60 ms from your baseline-you’re entering danger territory.
That delay doesn’t just sit there. It creates an electrical imbalance in your heart muscle, especially in the mid-layer of the ventricles (called M cells). This imbalance can spark early afterdepolarizations-tiny, abnormal electrical sparks that trigger a chaotic, fast heartbeat called Torsades de pointes. This isn’t just a flutter. It’s a cardiac emergency. If not treated immediately, it can turn into ventricular fibrillation and sudden death.
Not All Macrolides Are the Same
People often assume azithromycin is the safest macrolide because it’s prescribed more often. That’s true-but not because it’s harmless. It’s because it’s less risky than the others.
Here’s how they stack up in terms of QT prolongation risk:
- Clarithromycin: Highest risk. It blocks Ikr channels strongly and also inhibits CYP3A4, a liver enzyme that breaks down other drugs. This means it can raise levels of other QT-prolonging meds-like statins, antifungals, or antiarrhythmics-making the danger multiply.
- Erythromycin: Moderate risk. Less potent at blocking Ikr than clarithromycin, but it causes nausea and vomiting in up to 30% of users. That can lead to low potassium levels (hypokalemia), which alone doubles the risk of arrhythmias.
- Azithromycin: Lowest risk among macrolides-but still risky. Its Ikr blockade is weaker, and it barely affects CYP3A4. But large studies show it still increases cardiovascular death risk by nearly 3 per 1,000 courses, especially in the first five days of use.
Clarithromycin carries a black box warning in the U.S. for QT prolongation. Azithromycin has a warning, but no black box. That difference shapes how doctors prescribe them-even though both can be dangerous under the right (or wrong) conditions.
Who’s at Highest Risk?
For most healthy people, a short course of azithromycin is fine. But if you have even one or two risk factors, your chance of a bad outcome jumps dramatically.
Here are the six biggest red flags:
- Female sex: Women make up nearly 70% of all macrolide-induced TdP cases. Hormonal differences affect how potassium channels behave.
- Age over 65: Older hearts have less "repolarization reserve"-meaning less ability to handle electrical stress.
- Baseline QTc over 450 ms: If your ECG already shows a long QT, adding a macrolide can push you into danger. This increases risk nearly fivefold.
- Other QT-prolonging drugs: Taking even one other drug that prolongs QT-like certain antidepressants, antifungals, or antipsychotics-can double your risk. Add two or more, and it gets worse.
- Low potassium or magnesium: Hypokalemia triples the risk. This is why vomiting, diarrhea, or diuretics can turn a safe drug into a deadly one.
- Heart failure or structural heart disease: Damaged hearts are electrically unstable. In heart failure patients, macrolides increase TdP risk over threefold.
And here’s the scary part: up to 20% of people who develop TdP after taking these drugs have an undiagnosed inherited long QT syndrome. Their baseline ECG looks normal. Their blood work is fine. But their heart’s potassium channels are genetically flawed. A single dose of azithromycin is all it takes to trigger catastrophe.
What Should Doctors Do?
Guidelines from the American College of Cardiology and the Infectious Diseases Society of America are clear:
- Check a baseline ECG if you have two or more risk factors.
- Don’t prescribe macrolides if your QTc is over 470 ms (men) or 480 ms (women).
- Avoid macrolides entirely if you’ve had TdP before or have congenital long QT syndrome.
- Use alternatives like doxycycline, amoxicillin, or cefdinir when possible.
For patients on multiple QT-prolonging drugs, switching from clarithromycin to azithromycin isn’t enough. The safest move is to avoid macrolides altogether.
Some hospitals now use tools like the Macrolide Arrhythmia Risk Calculator (MARC), which weighs 12 factors-age, sex, kidney function, meds, electrolytes-to predict individual risk with 89% accuracy. Point-of-care ECG devices like the CardioCare QT Monitor can give real-time QTc readings in under a minute, making screening practical even in urgent care settings.
What About the COVID-19 Era?
During the pandemic, azithromycin was often paired with hydroxychloroquine as a supposed treatment for COVID-19. Both drugs prolong QT. Studies showed the combination pushed QTc up by an average of 26.2 milliseconds-enough to trigger arrhythmias in vulnerable patients. That’s not just a theoretical concern. Emergency departments saw spikes in arrhythmias during that time, and many were linked to this combo.
It’s a cautionary tale: when drugs are used outside their approved indications, especially in sick patients, the risks multiply fast.
What Should You Do?
If you’re prescribed a macrolide antibiotic:
- Ask your doctor: "Do I have any risk factors for heart rhythm problems?" Mention any history of fainting, family members who died suddenly under age 50, or unexplained seizures.
- Find out if you’re taking other drugs that affect your heart rhythm. Even over-the-counter antihistamines like diphenhydramine can add to the risk.
- Get a baseline ECG if you’re over 65, on diuretics, or have heart disease.
- If you feel dizzy, lightheaded, or notice your heart racing or skipping beats while on the antibiotic-stop taking it and get checked immediately.
Don’t assume your doctor already knows your full medical history. Many patients don’t mention past fainting spells or family cardiac deaths. But those details matter.
The Bigger Picture
Macrolide antibiotics saved lives for decades. But medicine evolves. We now know that a drug’s benefit isn’t just about killing bacteria-it’s about how it affects the whole body. The decline in clarithromycin use since 2020 shows the system working: doctors are learning, guidelines are updating, and patient safety is improving.
Still, over 10 million macrolide prescriptions are filled in the U.S. every year. That’s a lot of hearts at risk. The cost of monitoring? Around $14.30 per prescription. The cost of a cardiac arrest? Priceless.
The future may hold safer macrolides. Researchers are testing new versions like solithromycin, which blocks Ikr channels 78% less than clarithromycin. But until then, the safest approach is simple: know your risks. Ask questions. And don’t let convenience override caution.
Can azithromycin really cause heart problems?
Yes. While azithromycin has the lowest risk among macrolide antibiotics, it still carries a proven link to QT prolongation and Torsades de pointes. A 2012 study of over 1.3 million patients found a 2.85-fold increase in cardiovascular death during the first five days of azithromycin use compared to amoxicillin. The risk is small for healthy people but becomes significant with other risk factors like age, heart disease, or low potassium.
Is clarithromycin more dangerous than azithromycin?
Yes, significantly. Clarithromycin blocks the heart’s potassium channels more strongly than azithromycin and also inhibits liver enzymes that break down other medications. This means it can raise levels of other QT-prolonging drugs, creating a dangerous buildup. It carries a black box warning from the FDA, while azithromycin does not. For patients with multiple risk factors, clarithromycin should be avoided entirely.
What should I do if I’m already on a macrolide antibiotic?
If you’re taking a macrolide and have no risk factors, continue as directed. But if you have heart disease, are over 65, take other heart-affecting drugs, or have low potassium, talk to your doctor. Watch for symptoms like dizziness, palpitations, or fainting. If they occur, stop the medication and seek care immediately. Don’t wait for your next appointment.
Do I need an ECG before taking azithromycin?
Not always-but you should if you have two or more risk factors: age over 65, female sex, heart failure, low potassium, use of other QT-prolonging drugs, or a family history of sudden cardiac death. A simple 10-second ECG can catch a long QT before it becomes dangerous. Many clinics now offer point-of-care ECGs for under $20.
Are there safer alternatives to macrolide antibiotics?
Yes. For most respiratory infections, amoxicillin, doxycycline, or cefdinir are just as effective and carry no QT prolongation risk. For patients with penicillin allergies, alternatives like levofloxacin or linezolid may be options-but they come with their own risks. The key is to match the antibiotic to the infection and the patient’s health profile, not just convenience or habit.


Saurabh Tiwari
December 2, 2025 AT 15:06bro i took azithromycin last year for a bad cough and felt weirdly dizzy on day 3 🤔 didn't think much of it till i read this. now i'm kinda freaked out. my grandma had a pacemaker, maybe i should've gotten checked before popping those pills.
Shubham Pandey
December 2, 2025 AT 19:04macrolides are overprescribed. just give amoxicillin already.
Girish Padia
December 3, 2025 AT 09:54people these days want everything handed to them. if you're old or have heart issues, don't take antibiotics unless you're dying. stop being lazy and let your immune system work.
John Morrow
December 4, 2025 AT 11:35The pharmacodynamic profile of macrolide-induced hERG channel blockade is not trivial, particularly when co-administered with CYP3A4 inhibitors like ketoconazole or even grapefruit juice-both of which elevate plasma concentrations of clarithromycin beyond therapeutic thresholds. The QTc prolongation is not merely a statistical artifact; it's a clinically significant electrophysiological perturbation that disproportionately affects M-cells in the mid-myocardium, creating the substrate for re-entrant arrhythmias. The 2012 JAMA study you cited? It was a retrospective cohort with residual confounding. But the FDA’s post-marketing surveillance data from 2015–2020 confirms a 2.3-fold increased risk of sudden cardiac death in patients over 65 with concomitant diuretic use. We're not talking about rare outliers here-we're talking about preventable iatrogenic mortality in primary care settings where ECG screening remains underutilized due to systemic inertia and reimbursement barriers.
Elizabeth Farrell
December 4, 2025 AT 17:00This is such an important post. I’ve been a nurse for 18 years and I can’t tell you how many times I’ve seen patients dismissed because they ‘seem fine.’ One woman, 71, on hydrochlorothiazide, took azithromycin for bronchitis, and by day four she collapsed in the pharmacy. She had no prior history-just a normal ECG six months before. If we’d checked her potassium and QTc, we could’ve stopped it. Please, if you’re on diuretics, have a family history of sudden death, or are over 60-ask for the ECG. It takes 60 seconds. It could save your life. And doctors-you’re not doing your job if you’re not asking these questions. It’s not about being paranoid. It’s about being careful.
Anthony Breakspear
December 4, 2025 AT 19:16yo i used to think azithromycin was the safe one-turns out it’s just the ‘less dangerous’ option among drugs that shouldn’t be in your medicine cabinet unless you’re literally choking on bacteria. my uncle dropped dead after a Z-pack. they said it was ‘natural causes.’ nah. it was a silent potassium thief and a lazy doc who didn’t ask about his statins or his dad’s early heart attack. we gotta stop treating antibiotics like candy. get the ECG. check your meds. don’t let convenience kill you.
Kristen Yates
December 5, 2025 AT 15:11I didn't know this. I'm 68 and take a diuretic. My doctor gave me azithromycin last month. I'll call and ask about an ECG next week. Thank you for sharing this.
Saket Modi
December 6, 2025 AT 14:22another overhyped medical scare. next they'll say breathing is dangerous. 😴
John Webber
December 6, 2025 AT 21:47my doc gave me clarithromycin for sinus infection and i felt weird. i thought it was the cold. now i see i shoulda asked about my heart. i got a bad habit of not asking questions. my bad. i’ll do better next time.
Zoe Bray
December 8, 2025 AT 20:03It is imperative to underscore that the clinical management of macrolide-associated QT prolongation necessitates a comprehensive, risk-stratified approach grounded in evidence-based guidelines from the ACC and IDSA. The presence of two or more risk factors-including advanced age, female sex, electrolyte derangements, concomitant QT-prolonging medications, or structural heart disease-constitutes a Class IIa indication for pre-treatment electrocardiographic evaluation. Failure to implement point-of-care ECG screening in high-risk populations represents a significant gap in preventive cardiology and constitutes a potential deviation from the standard of care. Furthermore, the use of risk prediction tools such as the Macrolide Arrhythmia Risk Calculator (MARC) should be institutionalized in ambulatory and urgent care settings to mitigate preventable adverse cardiac events.