Ever felt like your pain is immune to over-the-counter painkillers? If so, you’re not alone. There’s a group of people out there who try all the usual NSAIDs—ibuprofen, naproxen, even diclofenac—yet their pain barely budges. When the “Big Three” NSAIDs don’t do the job, doctors sometimes turn to a medicine that’s not as well-known: indomethacin. It’s a bit like pulling out the big guns when everything else fails. So, why does this particular pill win where others fall flat? Prepare for a few surprises; indomethacin isn’t your average painkiller.
Why Indomethacin Is Different From Other NSAIDs
Most people know NSAIDs as the go-to for headaches or sore knees after a workout. But indomethacin isn’t sold in grocery stores right next to the gummy vitamins, and you won’t hear much about it unless you’re deep into the chronic pain trenches. This drug belongs in the same NSAID family, but it stands out with a punch that other members can’t always deliver. Indomethacin is particularly famous in the world of rare or stubborn pain syndromes—think gout flares, certain headaches like cluster headaches or hemicrania continua, and some tough cases of arthritis.
Unlike ibuprofen or naproxen, indomethacin is structurally different and a lot more potent. This extra strength doesn’t just mean better pain relief, but also a higher risk of side effects, so it’s not a first-line choice for most folks. Doctors reach for it when the pain truly refuses to budge. For example, if your joints swell and throb from gout and you’ve cycled through all the usual suspects, indomethacin often comes through when nothing else has worked.
Beyond that, neurologists sometimes see almost miraculous results for people with certain types of headaches. There’s even a specific term—“indomethacin-responsive headaches”—because some conditions, like paroxysmal hemicrania, just don’t budge without it. Think about that: the medicine is so effective for these pains that it actually changed the names of the conditions themselves.
But is there proof? Headache and rheumatology experts point to plenty of real-life data. For example, one study in "Cephalalgia" followed people with chronic head pain resistant to everything. When they were given indomethacin, a whopping 80% improved dramatically.
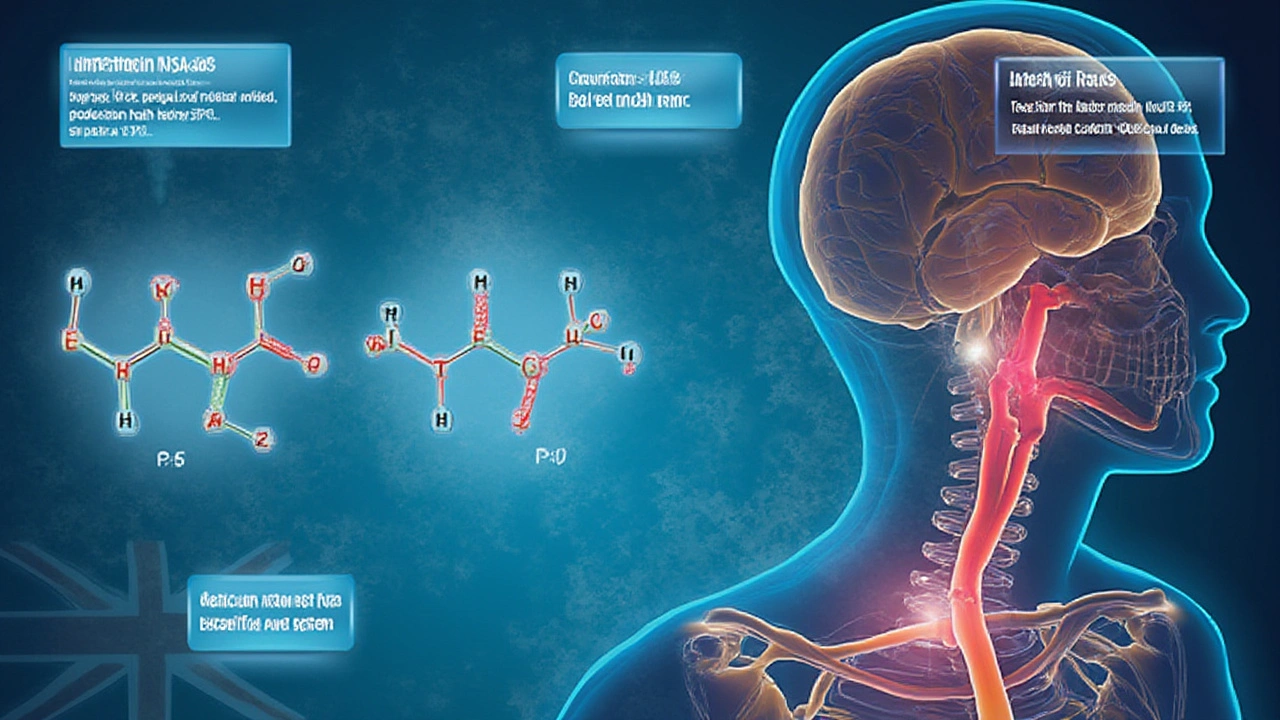
What’s behind all this? Indomethacin inhibits both COX-1 and COX-2 enzymes, which help make prostaglandins—the little molecules that tell your body to create inflammation and pain. That’s the same pathway other NSAIDs target, but indomethacin is way more powerful at shutting down this system. In short: when other options barely make a dent, indomethacin gets serious work done.
The Science: How Indomethacin Works in Chronic Pain
It’s easy to think of NSAIDs as all working essentially the same way. And yes, they’re all after those prostaglandins—blocking them to reduce swelling and pain. But with indomethacin, it’s a full-on roadblock, not just a speed bump. This potency explains why it can punch through chronic pain that laughs at other drugs.
Let’s break down the chain reaction: when cells in your body get hurt or inflamed, they release enzymes called COX-1 and COX-2. These enzymes help crank out prostaglandins, which sound like a group of friendly chemicals but actually cause swelling, redness, and pain. Indomethacin stomps on both COX-1 and COX-2, stopping those messages nearly at the source. As a side effect, though, it also blocks some of the good prostaglandins—like the ones that protect your stomach lining or keep your blood flowing steady.
So why is indomethacin so much better at this job? Chemically, it locks onto both enzymes tighter than most NSAIDs, so the effect is stronger and longer-lasting. It’s kind of like putting a clamp on a garden hose instead of pressing down with your thumb. In headache medicine, experts sometimes joke that if indomethacin doesn’t work, nothing else will.
One quirky thing stands out: indomethacin seems to have a special effect on inflammation that involves the brain and nerves—not just in joints or muscles. That’s what makes it a lifesaver for certain rare headaches. Animal studies even hint at it calming pain pathways deep inside the brainstem, which might explain this edge.
There’s a catch, though. Because indomethacin is so forceful, your body pays for it. People who take it long-term have to watch out for stomach bleeding, kidney strain, and even mood changes. Those prostaglandins it blocks do more than cause pain—they’re also involved in protecting your body. If you’re taking indomethacin for weeks or months, your doctor will want to run regular bloodwork and check-ups.
Want to see what conditions respond especially well? Here’s a quick rundown:
- Gout. Especially during sudden and severe flare-ups.
- Chronic inflammatory arthritis (sometimes when others fail).
- Cluster headaches and paroxysmal hemicrania.
- Ankylosing spondylitis (a rare spine arthritis).
If you’re curious about real patients’ stories and clinical data, this deep-dive into indomethacin and chronic pain pulls together some practical info and new insights.
Dosing Pearls: How to Use Indomethacin Safely
Indomethacin dosing isn’t just “take two and call me in the morning.” Even doctors tread carefully. Start too high, and you’re at higher risk for gut or kidney trouble. Start too low, and you might not touch the pain. So the art is in finding the lowest effective amount, and only ramping up if the pain stays stubborn.
The typical adult starting dose is around 25 mg two or three times per day with food. Some people, especially those with strong kidney or gut issues, might start even lower—maybe 25 mg once daily. In severe pain (like an acute gout attack), the dose might briefly go up to 50 mg three times daily, but only for a few days.
- Always take indomethacin with food or a full glass of water to protect your stomach.
- Never mix it with other NSAIDs (like ibuprofen or naproxen) unless told by a doctor—this seriously increases risk of side effects.
- Long-acting (sustained-release) forms are available. They’re handy if you need around-the-clock coverage, but can still hit the stomach just as hard.
- People with chronic kidney or liver issues might need lower, less frequent dosing. It’s not a medicine for daily headaches or non-specific joint pains.
Dosing for headaches usually starts low—sometimes even just a single 25 mg pill twice a day—to test if you’re sensitive to side effects. If it works and you can tolerate it, the doctor may bump up the dose, but rarely beyond 200 mg per day in divided doses.
It’s easy to get nervous about the risks, so here are some key things to watch for:
- Any sign of stomach pain, black/tarry stools, or vomiting blood—stop immediately and call the clinic. These are red flags for stomach bleeding.
- If you’re on blood thinners or have a history of ulcers, careful monitoring or a different drug may be better.
- Headache relief often shows up in the first few days. Gout and arthritis usually respond within a week.
- Some folks notice dizziness or confusion, so don’t drive or work around machinery until you know how you react to indomethacin.
- Avoid alcohol—it makes stomach and kidney side effects much more likely.
Rosalind, for instance, had a friend who switched to indomethacin for her mom’s relentless gout attacks. The difference was night and day…but only after her doctor carefully set the dose to match her kidney function. It pays to start slow and check in often with your clinic.
Side Effects and Monitoring Essentials
You’ve probably figured out by now that indomethacin is not a mild-mannered pain reliever. This is the honest truth: the side effects can be serious, especially if misused. Understanding what to look for can keep you out of trouble.
Here’s a breakdown of the main issues people run into:
- Stomach irritation (heartburn, ulcers, and bleeding) – even with careful use, up to 30% of people get at least some symptoms.
- Kidney strain – less common for short-term use, but long-term users can see their kidney function deteriorate. About 20% of long-term patients may show some drop in filtration rate.
- Mood changes or confusion – unique to indomethacin, especially in older adults. It can cause depression, agitation, or “brain fog.”
- High blood pressure – probably because of kidney effects.
- Fluid retention and potential swelling.
Doctors usually keep a close eye on patients using indomethacin for more than a few weeks. Here’s a quick table for how often things are checked:
| Test | When to Check |
|---|---|
| Kidney function (creatinine, BUN) | At baseline, then every 3-6 months |
| Liver tests | At baseline, then yearly |
| Blood pressure | Every visit |
| Signs of GI bleeding (blood in stool, anemia) | Every visit, or if symptoms arise |
There are tricks to lower risk:
- Take every dose with food.
- Ask about stomach-protecting pills (like omeprazole or other PPIs) if you’re prone to ulcers.
- Stay hydrated, but don’t overdo salt or anti-inflammatory diet fads that could throw off your labs.
- If you ever develop allergic reactions (rash, swelling, trouble breathing), stop and seek care. Allergy is rare but dangerous.
Real-world tip: be open with your doctor about any past stomach or kidney problems. Tell them if you’re taking diuretics, ACE inhibitors, or blood pressure meds—these can clash with indomethacin. For women who are pregnant, indomethacin is usually off-limits, especially late in pregnancy, as it can harm the baby’s circulation.
Docs rarely use indomethacin in kids, but if you see it on a pediatric prescription, ask questions right away. It’s reserved for special circumstances, like specific types of juvenile arthritis where nothing else works.
Thanks to its unique risks, many doctors are hyper-cautious about starting indomethacin without a recent blood panel and at least one check-in visit a month or two after the first prescription.
Practical Tips and What to Expect from Indomethacin
If you’ve slogged through months or years of chronic pain, new hope can seem too good to be true. Yet indomethacin has real street cred among pain specialists. If this is the drug your doctor recommends, you’ll want to get the most out of every pill while avoiding the pitfalls.
The first rule: set expectations. If your diagnosis is one of those rare headaches or stubborn arthritis types, a trial of indomethacin might bring relief no other NSAID can touch. But if your pain is non-inflammatory or you’re just chasing fatigue and muscle aches, don’t expect miracles—indomethacin isn’t a catch-all.
Another practical tip: write down your pain scores for a few days before and after starting the medicine. Bring that journal to your follow-up. Your provider will make dose tweaks based on this data, not just guesswork.
Some people notice results fast—sometimes in 24 hours for headaches or gout. More chronic conditions, like spondylitis, may need up to a couple of weeks for the full effect. If you get decent relief but can’t tolerate the side effects, ask if a lower dose combined with another therapy is safer.
Let’s bust one myth: long-term use isn’t always required. In some cases (especially bad gout or headache flares), people only need indomethacin for a few days or a week. Then it’s shelved until the next big attack. But for chronic, unrelenting pain, a steady schedule makes sense—as long as your labs look good.
Don’t skip blood work or ignore new symptoms, no matter how well the pain is controlled. Your stomach, kidneys, and blood pressure aren’t invincible, especially as you get older.
A good rapport with your provider—a shared understanding of your goals and fears—makes all the difference. If indomethacin works for you when nothing else has, it’s a game-changer. But that comes with big responsibilities, on both sides of the doctor–patient table.


Alex Hundert
July 24, 2025 AT 05:06Man, I’ve been on indomethacin for three years now for ankylosing spondylitis. Took me six months to find the right dose-25mg twice a day with food-and now I can actually walk without feeling like my spine’s made of rusted nails. Side effects? Yeah, I get heartburn sometimes. But I take omeprazole like it’s my morning coffee. Worth it.
Emily Kidd
July 25, 2025 AT 04:53i’ve been usin this for cluster headaches and holy hell it’s a miracle. i used to wake up at 3am like a human alarm clock screaming. now? i take one 25mg pill and i’m back to sleep. doc said if it works this good, it’s basically diagnostic. also, dont skip the stomach meds. i learned the hard way.
caiden gilbert
July 26, 2025 AT 08:30Indomethacin feels like the punk rock of NSAIDs-loud, chaotic, and totally out of place at a yoga retreat. You don’t take it because you want to, you take it because your body’s screaming and everything else just whispered back. I’ve seen people go from wheelchairs to walking dogs after starting it. But man, the side effects? That’s the price of admission. I keep a journal of every burp, every dizzy spell. It’s not a drug, it’s a relationship.
phenter mine
July 26, 2025 AT 16:16so i started indomethacin last month for my gout and it was like magic. like, i couldnt even tie my shoes and now i ran 5k. but my stomach has been on fire and i keep forgettin to take the omeprazole. i think i need to stop being lazy and actually follow the rules. also why is it called indomethacin? sounds like a villain in a superhero movie.
Callum Breden
July 27, 2025 AT 17:25This is a textbook example of pharmaceutical overreach. Indomethacin is a blunt instrument masquerading as precision medicine. The side effect profile is abysmal, and the fact that it's prescribed at all speaks to a systemic failure in pain management. You're trading organ damage for temporary relief. This isn't treatment-it's desperation dressed in a white coat. Anyone taking this long-term is either a martyr or dangerously uninformed.
Arrieta Larsen
July 28, 2025 AT 06:28I know people who’ve been on this for years and swear by it. But I also know one woman who ended up in the ER with a bleed after taking it with ibuprofen for a bad back. Please, if you’re thinking about trying it-talk to your doctor, get bloodwork done, and don’t treat it like a weekend warrior’s fix. Your body’s not a lab rat.
Kathy Pilkinton
July 29, 2025 AT 09:24Oh wow, another ‘miracle drug’ that’s basically just a chemical sledgehammer. Let me guess-next you’ll be telling me that opioids are just ‘stronger painkillers’ and we should all be on them. Indomethacin isn’t a solution, it’s a last resort for people who’ve been failed by the system. And yet here we are, glorifying it like it’s some kind of miracle. You don’t fix chronic pain by poisoning your stomach. You fix it by fixing the system.
Holly Dorger
July 30, 2025 AT 03:45I’m from a small town in Nebraska and our local pharmacist remembers every patient by name. When I told her I was starting indomethacin, she looked me dead in the eye and said, ‘You better be ready to live with this one.’ She handed me a little card with the warning signs printed in bold. I still have it taped to my medicine cabinet. Don’t underestimate how much care matters when you’re on something this heavy.
Amanda Nicolson
July 31, 2025 AT 07:24Let me tell you about the night I took my first 50mg of indomethacin for a gout flare-I was crying in the kitchen because my big toe felt like it was being slowly crushed by a steamroller, and then, three hours later, I woke up and thought it was morning and I was fine. Like, completely fine. No pain. No swelling. Just… quiet. I sat there for ten minutes just staring at my toe like it was a stranger who’d moved out. I cried again. Not from pain-from relief. That’s the kind of moment that makes you forget the stomach aches, the dizziness, the blood tests. That’s the kind of moment that makes you willing to risk it all.
Jackson Olsen
August 1, 2025 AT 17:44i tried it for a week for my knee. worked good. got dizzy. stopped. no regrets. if it works for you cool. if not dont force it. also dont mix with other pills. i learned that from a guy on the bus.
Penny Clark
August 3, 2025 AT 11:50My mom’s been on this for 8 years for rheumatoid arthritis. She takes it with yogurt and a banana every time-says it helps. She checks her BP every morning and writes it down in this little notebook she calls her ‘pain diary.’ She doesn’t talk about it much, but I’ve seen her smile when she walks without her cane. It’s not perfect, but it’s hers. And sometimes that’s enough.
Niki Tiki
August 4, 2025 AT 17:47Why are we even talking about this? In America we just throw pills at problems instead of fixing why people are in pain in the first place. You think indomethacin is the answer? Try paying rent. Try not working 60 hours a week. Try having healthcare. But nope, let’s just give someone a chemical sledgehammer and call it progress. This isn’t medicine-it’s capitalism with a prescription pad.
Jim Allen
August 6, 2025 AT 07:55indomethacin is basically the universe’s way of saying ‘you’ve been too soft on pain.’ it doesn’t care if you’re scared or tired or broke. it just says ‘here, feel nothing for now, but pay later.’ and honestly? kinda poetic. we all want to be numb sometimes. this just makes it legal.
Nate Girard
August 7, 2025 AT 03:50My cousin’s neurologist prescribed this for her hemicrania continua and it was like flipping a switch. She hadn’t slept through the night in two years. Now she’s training for a marathon. But she’s also on monthly blood tests, PPIs, and a strict no-alcohol rule. It’s not magic-it’s management. And that’s okay. Sometimes the best treatments are the ones that demand responsibility.
Carolyn Kiger
August 7, 2025 AT 14:59I used to think pain meds were just about strength. Then I met someone on a support forum who’d been on indomethacin for 15 years. She told me the real trick isn’t the dose-it’s the rhythm. Taking it at the same time every day. Eating before. Tracking sleep. Talking to her doctor every time she felt off. It’s not a pill. It’s a daily ritual. And that’s what kept her alive.
krishna raut
August 7, 2025 AT 23:47Works for gout. Avoid if kidney issues. Simple.
Prakash pawar
August 8, 2025 AT 04:28Indomethacin is the only true warrior in the battlefield of chronic pain. While ibuprofen plays with toys, indomethacin marches into the fire and drags your suffering out by the collar. Modern medicine is afraid of power. They want gentle solutions. But pain doesn’t care about gentleness. It demands a reckoning. And indomethacin? It answers the call. The side effects are not flaws-they are the cost of truth.
Alex Hundert
August 9, 2025 AT 07:36Just read your comment about the ‘cost of truth’-I get it. But truth doesn’t come with a stomach ulcer. My doc told me last month my gastric lining is paper-thin. I’m not fighting pain anymore. I’m just trying not to bleed out. Indomethacin saved my mobility. But it’s also the reason I now take 5 pills just to stay alive. That’s not philosophy. That’s survival.