Automated Dispensing Cabinets (ADCs) are meant to make medication delivery faster and safer in clinics and hospitals. But if they’re not set up and used right, they can actually cause more mistakes than they prevent. In fact, one study found that in six out of seven nursing units, medication errors went up by more than 30% after ADCs were installed. That’s not because the technology is flawed-it’s because people skipped the basics. Getting ADCs right isn’t about buying the most expensive model. It’s about how you train staff, configure the system, and enforce rules.
Why ADCs Can Make Things Worse
ADCs look like high-tech lockers with touchscreens and barcode scanners. They’re supposed to stop the wrong drug from being given to the wrong patient. But if a nurse scans the wrong barcode because the fentanyl and naloxone drawers are right next to each other, the system won’t catch it. If override buttons are left wide open, staff can grab any drug without pharmacist approval. And if restocking isn’t done carefully, look-alike, sound-alike drugs like hydromorphone and morphine end up in the same drawer.
These aren’t hypothetical risks. In 2017, a patient received 10 times their prescribed insulin dose because the ADC was programmed to allow high-dose vials without a second check. The cabinet didn’t fail-the people using it didn’t follow safety steps. The Institute for Safe Medication Practices (ISMP) says ADCs don’t improve safety unless the design and use are planned with patient profiling in mind. That means the system needs to know who the patient is, what drugs they’re on, and what allergies they have before anything is dispensed.
Core Safety Rules You Can’t Skip
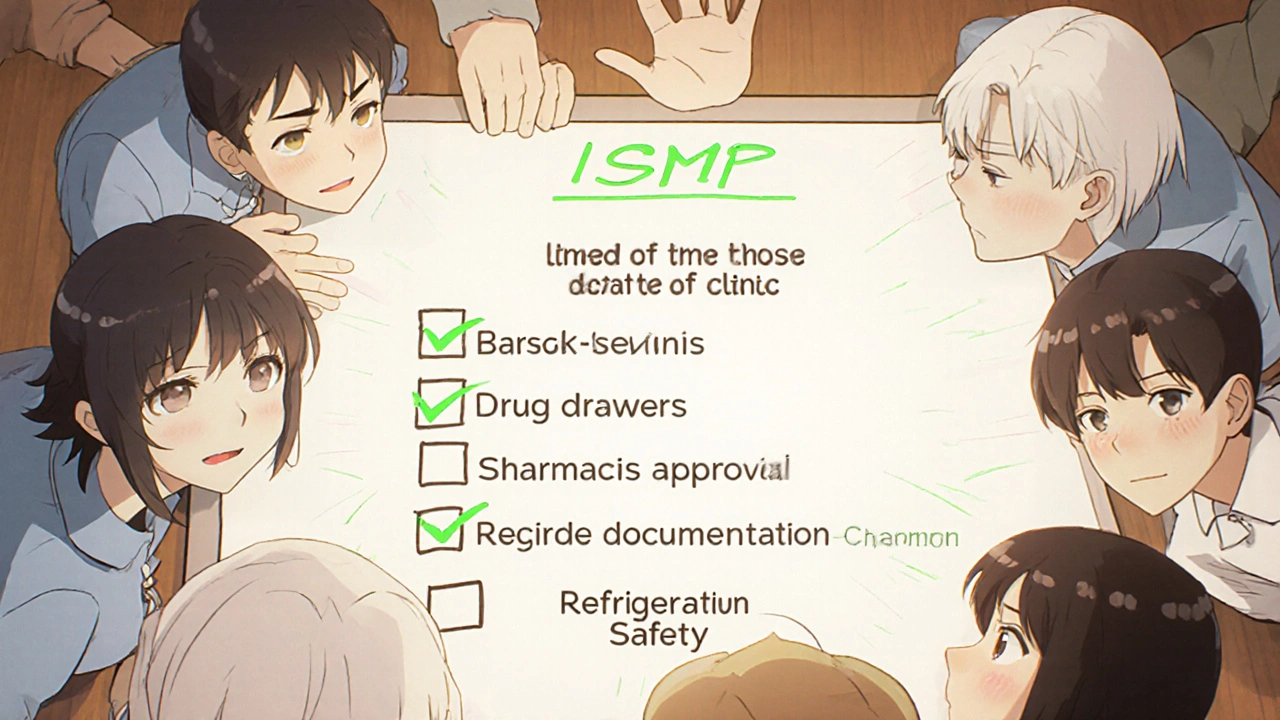
The ISMP published nine Core Safety Processes in 2019 that every clinic using ADCs must follow. You don’t need to memorize all of them, but here are the five that matter most:
- Require barcode scanning for every medication taken out. No exceptions. Even if you’re in a rush, scanning the patient’s wristband and the drug barcode is your last line of defense. Systems like BD Pyxis and Omnicell XT can be set to block dispensing if the scan doesn’t match.
- Lock down override functions. Overriding the system to grab a drug without approval should be rare. One study showed facilities with unrestricted overrides had 2.3 times more errors. Create unit-specific override lists-only allow access to drugs that are truly needed in emergencies, like epinephrine or naloxone. And every override must be documented with a reason and signed off by a second licensed provider.
- Separate look-alike, sound-alike drugs. Don’t put insulin glargine next to insulin lispro. Don’t put hydromorphone next to morphine. Use physical barriers, different drawer colors, or even separate cabinets. One clinic reduced look-alike errors by 68% just by moving these drugs apart.
- Ensure pharmacist review before dispensing. If your ADC isn’t connected to your pharmacy system, you’re missing the biggest safety net. Pharmacists need to review all orders before the cabinet releases medication. Without this, nurses won’t get alerts about duplicate therapy, dangerous interactions, or incorrect doses.
- Keep refrigerated meds properly stored. Vaccines, insulin, and certain antibiotics need to stay cold. The ISMP says refrigerated compartments must be away from computer screens and other heat sources. And every vial must have a beyond-use date (BUD) clearly labeled. A 2021 audit found 22% of clinics had expired meds in their ADCs because labels weren’t updated.
Choosing the Right ADC for Your Clinic
Not all cabinets are built the same. If you’re a small clinic, you don’t need a full-size unit that costs $40,000. Capsa Healthcare’s 4T countertop model is designed for ambulatory settings and costs under $20,000. It’s compact, integrates with EHRs via HL7, and supports barcode scanning. For larger clinics or hospitals, Omnicell’s XT Series or BD Pyxis MedStation offer more storage and advanced features like AI-powered diversion detection.
Here’s what to compare:
| Model | Price Range | Key Safety Features | Best For |
|---|---|---|---|
| Capsa NexsysADC | $15,000-$35,000 | Barcode scanning, EHR integration, temperature zones | Small clinics, outpatient centers |
| Omnicell XT | $25,000-$45,000 | AI diversion alerts, voice prompts (coming 2024), biometric login | Hospitals, ICUs |
| BD Pyxis MedStation | $30,000-$50,000 | Enhanced barcode verification, return medication tracking | High-volume units, surgical centers |
Don’t just pick the cheapest. Look at how well it connects to your electronic health record (EHR). If it doesn’t talk to your EHR, you’re losing the biggest benefit: real-time alerts for allergies, drug interactions, and incorrect dosing.
Training and Competency Matter More Than Technology
Most clinics spend thousands on ADCs but only a few hours training staff. That’s a recipe for disaster. Nurses need to understand not just how to scan a barcode, but why the system blocks certain actions. A 2021 survey found 42% of nurses felt their cognitive load increased because they had to manage overrides, confirmations, and alerts all at once.
Here’s how to train properly:
- Start with a 4- to 6-week competency program. Don’t let anyone use the cabinet until they’ve passed a hands-on test.
- Use real scenarios. Show them how a mis-scan could lead to a fatal error. Role-play override situations.
- Include pharmacists in training. They need to know how to review logs and spot patterns of misuse.
- Re-train every 6 months. New staff come in. Software updates happen. Safety habits fade.
At Mayo Clinic, they reduced override-related errors by 63% after implementing unit-specific training and weekly safety huddles. That’s not magic-that’s consistency.
What to Do When Things Go Wrong
Even the best systems fail. When an error happens, don’t just blame the nurse. Ask: Why did this happen? Was the cabinet misconfigured? Was the drug restocked incorrectly? Was the override used without documentation?
Set up a simple reporting system:
- Log every near-miss and actual error in a shared tracker.
- Review them weekly with pharmacy, nursing, and IT.
- Change one thing at a time. If multiple nurses are scanning the wrong drawer, maybe the labels need to be bigger. If overrides are too common, maybe the list needs to be tighter.
- Share successes. If a nurse caught a wrong drug before administration, celebrate it. Positive reinforcement works better than punishment.
One clinic reduced dispensing errors by 40% in six months just by reviewing logs and adjusting drawer layouts. They didn’t buy new equipment. They just listened to their staff.
Future Trends and What to Watch For
ADC technology is getting smarter. Omnicell is rolling out voice-activated interfaces in 2024. BD Pyxis plans biometric login (fingerprint or facial recognition) by 2025. HL7 FHIR integration-real-time data sharing with EHRs-is expected to grow from 35% to 78% of installations by 2026.
But the biggest trend isn’t tech. It’s standardization. Right now, only 63% of facilities follow all nine ISMP Core Safety Processes. That’s a problem. As more clinics adopt ADCs, the industry needs to agree on what “safe” means. Until then, your clinic’s safety depends on your team’s discipline-not the brand of cabinet you bought.
Final Checklist for Safe ADC Use
Before you turn on your ADC, run through this:
- ☑ Is the system connected to the EHR and pharmacy system?
- ☑ Are all medications scanned before and after dispensing?
- ☑ Are look-alike/sound-alike drugs physically separated?
- ☑ Are override functions limited, documented, and witnessed?
- ☑ Are refrigerated meds stored away from heat sources with clear BUD labels?
- ☑ Has every staff member completed training and passed a competency test?
- ☑ Are override logs reviewed weekly?
- ☑ Is there a disinfectant wipe station next to the cabinet?
If you can answer yes to all eight, you’re ahead of most clinics. If not, fix one thing this week. Don’t wait for the next audit. Medication errors don’t wait.
Can automated dispensing cabinets reduce medication errors?
Yes-but only if they’re set up and used correctly. Studies show ADCs can reduce dispensing errors by 15-20% when integrated with pharmacy review and barcode scanning. But if overrides are unchecked or drugs are misloaded, errors can increase by over 30%. The cabinet doesn’t fix bad processes-it exposes them.
What’s the biggest mistake clinics make with ADCs?
The biggest mistake is assuming the technology alone is enough. Clinics often buy an ADC, plug it in, and expect safety to improve automatically. But without pharmacist oversight, proper training, and strict override controls, the cabinet becomes just another way to give the wrong drug faster.
How often should ADCs be audited?
Audit the cabinet at least monthly. Check for expired medications, incorrect restocking, unused override logs, and misplaced drugs. Some clinics do weekly spot checks on high-risk items like opioids and insulin. Use the ISMP’s free ADC self-assessment tool to guide your audits.
Do I need a pharmacist to approve every medication from the ADC?
For scheduled medications, yes. The Joint Commission and ASHP recommend pharmacist review before dispensing. Emergency overrides are allowed, but they must be documented and reviewed afterward. If your system doesn’t require pharmacist approval, you’re skipping the most important safety layer.
Are ADCs worth the cost for small clinics?
If you dispense more than 50 different medications per week, yes. Even small clinics can benefit from reduced waste, better control over controlled substances, and fewer errors. The Capsa 4T model starts under $15,000 and fits on a countertop. The real cost isn’t the machine-it’s the cost of a single medication error.


Conor McNamara
November 18, 2025 AT 23:02they say adc's reduce errors but i've seen the logs... every override gets buried under 3 layers of bureaucracy. someone's selling these things to hospitals and whispering 'it's all automated now' while the nurses are drowning in pop-ups. i swear half the time the barcode scanner reads the damn coffee cup instead of the vial.
Leilani O'Neill
November 20, 2025 AT 20:33Let me be clear: this isn’t about technology. It’s about the erosion of professional standards. Nurses today are trained to click, not to think. The moment you let someone bypass a safety protocol because they’re ‘in a rush,’ you’ve already lost. This isn’t a cabinet issue-it’s a cultural rot.
Riohlo (Or Rio) Marie
November 21, 2025 AT 12:58Oh sweet mercy, another tech-utopian manifesto wrapped in ISMP jargon. You know what’s really dangerous? The fact that we’ve outsourced clinical judgment to a touchscreen that doesn’t care if you’re hungover, grieving, or just plain exhausted. The real villain isn’t the cabinet-it’s the system that treats nurses like glorified vending machine attendants. And don’t even get me started on the ‘beyond-use date’ labels that fade after three weeks. Someone’s clearly never held a vial of insulin in a 98°F storage closet while a code blue screams down the hall.
steffi walsh
November 22, 2025 AT 16:44Thank you for this. I’ve been saying this for years. I work in a small clinic and we got our Capsa 4T last year. The training took 6 weeks, we did role-plays with fake meds, and now we have a weekly huddle. Last month, a nurse caught a duplicate warfarin order because the system flagged it. We celebrated with donuts. Small wins matter.
Girish Pai
November 23, 2025 AT 03:38Let’s be real-this is a Western problem. In India, we use manual logs, handwritten scripts, and pharmacists who know every patient by name. No barcode? No problem. No AI? We don’t need it. Our error rate is lower because we don’t outsource responsibility to machines. Tech is a crutch for lazy systems.
Kristi Joy
November 23, 2025 AT 12:04I love how this article doesn’t blame the nurses. So many places treat ADCs like magic boxes and then punish the person who presses the wrong button. But the truth? If the system isn’t intuitive, if the drawers aren’t labeled clearly, if the alerts are too noisy-it’s not the nurse’s fault. It’s design failure. Let’s fix the system, not the staff.
Hal Nicholas
November 25, 2025 AT 10:21They’re lying. Every single one of them. ADCs are surveillance tools disguised as safety devices. The real goal? Track every move you make. Who overrode? Who scanned late? Who took insulin at 2 AM? They’re building a digital cage. And you’re applauding the lock.
Louie Amour
November 27, 2025 AT 01:59Wow. You actually think a $15,000 countertop unit is ‘safe’? That’s like putting a bike lock on a bank vault. If you’re not using Omnicell XT with biometric login and AI diversion detection, you’re not just negligent-you’re actively endangering lives. And don’t get me started on those ‘competency tests’-half the nurses can’t spell ‘hydromorphone.’
Kristina Williams
November 27, 2025 AT 05:51My cousin works at a hospital and says the ADCs are rigged. They program them so you can’t take more than 2 doses of fentanyl unless the pharmacy approves it... but the pharmacy is always asleep. So they just take it from the crash cart. No one knows. No one cares. The system is broken. I told my sister to quit nursing.
Shilpi Tiwari
November 28, 2025 AT 21:14From a clinical informatics perspective, the real bottleneck is HL7 FHIR interoperability. Without real-time EHR integration, the ADC becomes a siloed data sink. The ISMP guidelines are foundational, but the architectural dependency on HL7v3 vs. FHIR is the hidden variable in error reduction metrics. Most institutions still rely on legacy interfaces that don’t support dynamic patient profiling. That’s why override rates remain high-it’s not culture, it’s protocol.
Christine Eslinger
November 29, 2025 AT 00:44Here’s what I’ve learned after 18 years in med-surg: machines don’t save lives. People do. But people need space to think, not just scan. The best ADC isn’t the one with the most sensors-it’s the one that lets a tired nurse pause, breathe, and say ‘wait, something’s off.’ That’s why training matters more than tech. And why we need to stop treating safety like a checklist. It’s a mindset. It’s a habit. It’s the quiet moment between the beep and the button. That’s where the magic happens.