More than half of adults over 65 take five or more medications daily. For many, that means juggling pills at breakfast, lunch, dinner, and bedtime-with some requiring empty stomachs, others needing food, and a few only at night. It’s no wonder so many miss doses or take the wrong pill. The good news? Medication simplification isn’t just possible-it’s proven to help older adults stay independent, safer, and more in control of their health.
Why Complex Medication Regimens Are a Problem
It’s not just about too many pills. It’s about timing. A typical regimen might include:
- Levothyroxine on an empty stomach, 30 minutes before breakfast
- Metformin with breakfast and dinner
- Atorvastatin at bedtime
- Losartan in the morning
- Aspirin after lunch
- Acetaminophen as needed for pain
- Three different eye drops at different times
That’s seven different times a day to remember. Add in a pill organizer with 28 compartments, and it’s easy to see why confusion sets in. Studies show that when older adults have more than four daily doses, adherence drops sharply. And when they miss doses, hospitalizations go up-especially for heart failure, diabetes, and high blood pressure.
But here’s the thing: most of these medications aren’t actually being taken correctly-not because the person doesn’t care, but because the system is too complicated.
What Medication Simplification Actually Means
Simplification doesn’t mean stopping meds. It means making them easier to take-without losing their benefit. There are three main ways this happens:
- Combining pills into one tablet (like a pill that has both a blood pressure and cholesterol drug)
- Switching to once-daily versions (like switching from twice-daily metoprolol to once-daily metoprolol succinate)
- Aligning doses with daily routines (like grouping all morning meds together)
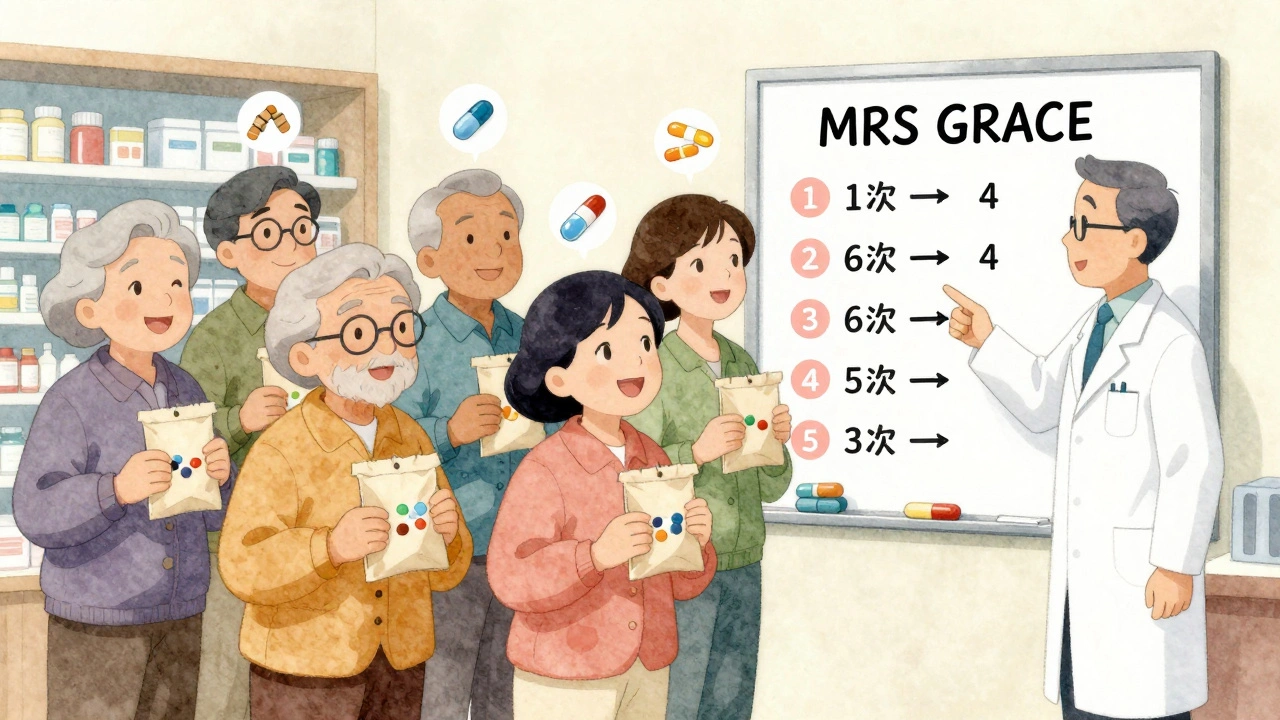
One study in Australian aged care homes found that 58% to 60% of residents had regimens that could be simplified using a simple five-question tool called MRS GRACE. The biggest win? Changing when pills were taken-not always changing the pills themselves.
For example, if someone takes a diuretic at night, they might wake up to use the bathroom three times. Switching it to the morning reduces sleep disruption and makes it easier to remember. Same drug. Better timing.
What Works Best-and What Doesn’t
Not all medications respond the same way to simplification. Some are more flexible than others.
Good candidates for simplification:
- High blood pressure meds (many now come in once-daily forms)
- Cholesterol-lowering drugs (like statins-most can be taken anytime, even with food)
- Diabetes pills (some can be switched to once-daily extended-release versions)
- Antidepressants and antipsychotics (long-acting versions exist and reduce dosing frequency)
Tricky cases:
- Levothyroxine (must be taken alone, on an empty stomach, 30 minutes before food)
- Insulin (timing matters for blood sugar control)
- Some antibiotics (need strict timing to stay effective)
Here’s the catch: even when simplification improves adherence, it doesn’t always mean better health outcomes. Why? Because older adults often have multiple conditions. Taking a pill on time doesn’t fix a poor diet, lack of exercise, or untreated depression. But it does remove one big barrier to staying well.

The Step-by-Step Process
Real simplification isn’t a quick fix. It’s a careful process. Here’s how it works in practice:
- Get the full list-not what the person remembers, not what’s on the bottle. A pharmacist or GP should compile a ‘best possible medication history’ by checking prescriptions, hospital records, and even over-the-counter meds. On average, people have six errors or omissions in their medication list.
- Check what’s still needed-some meds may no longer be necessary. Maybe a painkiller was prescribed for a back injury that healed years ago. Maybe a blood thinner is no longer needed after a heart procedure. This step is called deprescribing.
- Look for combo pills-ask if there’s a single tablet that combines two drugs. For example, a combo of lisinopril and hydrochlorothiazide replaces two separate pills.
- Switch to once-daily versions-many meds now have extended-release forms. Ask if the current version can be changed.
- Group by time of day-move all morning meds to one time, all evening meds to another. Even if you can’t reduce the number of pills, reducing the number of times you take them makes a huge difference.
This whole process usually takes 30 to 60 minutes per person. That’s why many GPs don’t do it-they’re pressed for time. But pharmacists, especially those trained in geriatric care, are the best people to lead this.
Real Impact: What Happens When You Simplify
In a 2020 study of community-dwelling older adults in the U.S., 41% of medication regimens were successfully simplified just by reducing how many times a day pills had to be taken. In Australian aged care homes, staff reported a 30% drop in medication errors after using the MRS GRACE tool.
One woman in Perth, 78, was taking 14 different medications across six times a day. After a pharmacist review, she was switched to:
- One combo pill for blood pressure and cholesterol (morning)
- One once-daily diabetes pill
- One daily aspirin
- One levothyroxine (still on empty stomach, but now just one pill)
She went from 14 pills, six times a day, to 4 pills, two times a day. She started taking them regularly. Her blood pressure improved. She didn’t have to refill her pill box every week. And she said, ‘I finally feel like I’m in charge again.’
Who Should Be Doing This?
It’s not just the doctor’s job. It’s a team effort:
- Pharmacists are the experts in medication timing, interactions, and alternatives. They’re trained to spot simplification opportunities.
- General practitioners need to refer patients for medication reviews, especially if they’re on five or more meds.
- Family caregivers can help by tracking what pills are taken, when, and whether side effects appear.
- The person taking the meds needs to be part of the conversation. Do they prefer to take everything in the morning? Do they hate swallowing pills? Their preferences matter.
There’s a tool called MRS GRACE that’s now used in Australia and being adopted in the U.S. and Europe. It’s not software-it’s a simple five-question checklist:
- Can any doses be moved to the same time of day?
- Are there combination products available?
- Can any medications be switched to once-daily forms?
- Are any medications no longer needed?
- Has the patient’s ability to manage meds changed?
Healthcare providers can learn it in under two hours. But most still don’t use it-because no one’s asking them to.
Barriers and How to Overcome Them
Even though simplification works, it’s not common. Why?
- Time-most GP visits are 10 minutes. A full med review takes 45.
- Cost-in many places, pharmacists aren’t paid to do these reviews.
- Training-only 35% of pharmacy schools teach this skill.
- Assumption-many doctors assume older adults can handle complexity, or that they’ll just ‘figure it out.’
Here’s how to push for change:
- Ask your pharmacist: ‘Can you do a medication review?’
- Ask your GP: ‘Is there a simpler way to take these?’
- Use a pill organizer with alarms or a smartphone app (like Medisafe or MyTherapy) to track what’s taken.
- Bring all meds-bottles, supplements, creams-to every appointment.
And if you’re a caregiver: don’t assume the person is taking their meds correctly. Watch them. Ask them to show you. It’s not about distrust-it’s about safety.
What’s Next?
Technology is catching up. Electronic health records now include tools that flag complex regimens. Epic Systems, one of the biggest health record platforms, has a feature that scores how complicated a patient’s regimen is and suggests simplifications.
But tech alone won’t fix this. It needs people-trained, paid, and empowered-to do the work. In Germany, pharmacists get paid extra for doing these reviews. In Australia, the government is pushing for it to be part of standard aged care. In the U.S., Medicare Advantage plans are starting to reward providers who reduce hospital readmissions linked to medication errors.
The goal isn’t to cut pills. It’s to cut confusion. To give older adults back their time, their dignity, and their independence.
Medication simplification isn’t a luxury. It’s a necessity for an aging world. And it starts with one question: ‘Is there a simpler way?’
Can I just stop some of my meds if I feel overwhelmed?
No. Stopping medications without medical advice can be dangerous. Some drugs, like blood pressure or seizure meds, need to be tapered slowly. Others, like statins or antidepressants, can cause rebound effects. Always talk to your doctor or pharmacist first. They can help you decide what’s safe to stop, adjust, or simplify.
Are combination pills as effective as taking them separately?
Yes, if they’re made correctly. Combination pills contain the same active ingredients as the separate pills, just in one tablet. They’re tested to ensure the same absorption and effect. The only downside is less flexibility-if you need to adjust one drug, you may have to switch the whole combo. But for most people, the benefit of fewer pills outweighs this.
What if my meds need to be taken at specific times for medical reasons?
Some meds do need precise timing-like levothyroxine (must be taken before food) or certain antibiotics. But even then, you can often group other meds around them. For example, if you take levothyroxine at 7 a.m., you can take all your other morning pills at 7:30 a.m. after the 30-minute window. The goal isn’t to ignore medical rules-it’s to work within them to reduce daily complexity.
How do I know if my current meds can be simplified?
If you take five or more medications daily, or if you have more than four doses per day, you’re a strong candidate. Ask your pharmacist to review your list. Bring all your bottles-including vitamins and supplements. They’ll check for duplicates, outdated prescriptions, and opportunities to combine or switch to once-daily versions. You don’t need a referral-just ask.
Will simplifying my meds save me money?
Sometimes. Combination pills are often cheaper than buying two separate ones. Once-daily versions may cost more per pill, but you’ll buy fewer pills overall. More importantly, fewer missed doses mean fewer hospital visits and emergency care, which can save thousands. Ask your pharmacist about cost comparisons before making changes.
Can I use a pill organizer to simplify my regimen?
Pill organizers help with memory, but they don’t reduce complexity. If you’re still taking 12 pills at five different times a day, a 7-day organizer just makes the mess bigger. True simplification means fewer pills and fewer times to take them. Use organizers as a backup-not a solution.
What if my doctor says my regimen is fine as it is?
It’s okay to ask for a second opinion. You can say: ‘I’m finding it hard to keep up with all these pills. Is there a simpler way that still keeps me safe?’ Many doctors don’t realize how complex regimens have become. A pharmacist can also provide a written summary of simplification options to bring back to your doctor.


Shubham Pandey
December 1, 2025 AT 23:46Too many pills. Too many times. Just give me one pill once a day. Why is this so hard?
John Webber
December 2, 2025 AT 20:25my grandma takes 12 pills and she forgets half of em. she just eats em all at breakfast now. doctor said its fine. she aint in no hospital yet.
Sandi Allen
December 4, 2025 AT 05:20Let me guess-this is another government-funded ‘simplify meds’ scam. Next they’ll tell us to stop taking insulin because ‘it’s too complicated.’
Who’s behind this? Big Pharma? The AMA? The WHO? They want us dependent on their pills-then they ‘simplify’ them into one super-pill that’s 3x more expensive. Don’t fall for it.
Elizabeth Farrell
December 4, 2025 AT 21:52I’ve been helping my 82-year-old neighbor with her meds for two years now. She was taking 17 pills across 8 different times a day. We worked with her pharmacist, used the MRS GRACE checklist, and now she’s down to 5 pills at two times. She cried when she said, ‘I finally have time to sit on my porch and read.’
It’s not just about pills-it’s about dignity. She didn’t need more medicine. She needed less chaos.
Saket Modi
December 6, 2025 AT 19:30lol another ‘simplify’ article. yeah right. i took my grandpa’s pills once. he had 27 different ones. i gave up after 3 minutes. someone else deal with it. 😩
william tao
December 7, 2025 AT 21:55While the article presents a superficially appealing narrative, it fails to address the underlying pharmacodynamic heterogeneity of polypharmacy in geriatric populations. The conflation of adherence with clinical efficacy is a dangerous reductionism. One must consider the risk-benefit calculus of deprescribing in the context of multimorbidity, frailty indices, and residual confounding from observational studies. The MRS GRACE tool, while elegant, lacks validation in diverse socioeconomic cohorts. The assumption that simplification universally improves outcomes is not evidence-based-it is aspirational.
Paul Santos
December 8, 2025 AT 19:21Ah yes, the eternal quest for ‘simplification’-as if life itself weren’t already a chaotic, beautiful mess. 🤔
But let’s be real: the real problem isn’t the pills-it’s the system that treats elders like broken machines needing firmware updates. We’ve outsourced care to algorithms and pill organizers while forgetting that humans need rhythm, not schedules. A once-daily pill is nice… but what about the quiet morning coffee with a daughter who remembers which pill is which? That’s the real medicine.
Eddy Kimani
December 10, 2025 AT 07:02Interesting data on adherence dropping after 4 daily doses. But I’m curious-has anyone looked at the pharmacokinetic impact of grouping meds? For example, combining statins with food might alter bioavailability, even if guidelines say it’s ‘fine.’ Also, what about drug-drug interactions when you stack 3 antihypertensives at once? The paper doesn’t mention CYP450 metabolism or renal clearance changes in elderly patients. Just saying-simplification needs pharmacological rigor, not just convenience.
Chelsea Moore
December 10, 2025 AT 10:32THIS IS WHY OUR ELDERLY ARE DYING IN SILENCE!!!
They’re too scared to say they’re confused! Too proud to admit they can’t read the tiny labels! Too alone to ask for help! And now we’re just giving them ‘combo pills’ like they’re a vending machine?!!
Where are the nurses? The home visits? The TRAINING for caregivers?!
They’re not ‘complex regimens’-they’re SYSTEMIC FAILURE!!!
John Biesecker
December 10, 2025 AT 23:37you know what’s wild? the fact that we think a pill is the solution to everything. 🌱
what if the real fix is less medicine and more walks? more meals with family? more sleep? more listening?
we treat aging like a bug to be patched, not a season of life to be honored.
maybe the simplest thing isn’t the pill-it’s the person who remembers to ask, ‘how are you today?’
Genesis Rubi
December 12, 2025 AT 08:29USA is falling apart. In my day, people took their pills like adults. Now we need apps, checklists, and ‘pharmacist reviews’ just to swallow a vitamin? This is why we lost the war on drugs. Weakness disguised as compassion.
Doug Hawk
December 12, 2025 AT 23:40My dad was on 11 meds. We did the full review. Turns out three were for conditions he no longer had. One was a duplicate. One was causing his dizziness. We cut five. He’s been more alert in 6 months than in the last 5 years.
But here’s the thing: the doctor never asked if he was having trouble. No one ever asked. We had to force it. That’s the real problem. We assume they’re fine. They’re not.
John Morrow
December 13, 2025 AT 13:35Let’s be brutally honest: medication simplification is a band-aid on a hemorrhage. The real issue is that we’re keeping people alive longer with chronic disease, while failing to invest in preventive care, social support, or geriatric training. We’re not simplifying regimens-we’re outsourcing the burden to families and pharmacists while pretending it’s a ‘solution.’
The real cost? The erosion of human connection. The pill organizer can’t replace a daughter who sits with her mother and says, ‘I’ll help you take them.’
Saravanan Sathyanandha
December 15, 2025 AT 12:59In India, we have a word: ‘jugaad’-a clever, low-cost fix. My aunt takes her thyroid pill before tea, her blood pressure pill after lunch, and her painkiller only when she can’t stand it. She doesn’t have a pillbox. She has a rhythm. She has her sons reminding her. She has her chai.
Maybe the answer isn’t more tech or combo pills-but more presence. More love. More time. Medicine is not just chemistry. It’s culture.
Elizabeth Farrell
December 17, 2025 AT 08:25Elizabeth here-just wanted to add: I’ve seen people go from needing help to open bottles to doing it all themselves after simplification. It’s not just about health-it’s about pride. One man told me, ‘I didn’t know I could still be the one in charge.’ That’s the quiet victory we’re not talking about.