When you’re over 70, taking the same dose of a medication you’ve used for decades can become dangerous-not because the drug changed, but because your kidneys didn’t keep up. As we age, kidney function naturally drops. By age 80, most people have lost nearly 40% of their kidney filtering capacity compared to their 30s. Yet, many doctors still use the same dosing rules for seniors as they do for younger adults. That’s how people end up in the hospital with confusion, falls, or even kidney failure from a simple prescription. The good news? You can prevent this. Monitoring kidney function isn’t just a lab test-it’s the key to safe, effective medication use in older adults.
Why Kidney Function Matters More After 70
Your kidneys don’t just make urine. They clean your blood. About 30% of all common medications-like painkillers, blood pressure pills, antibiotics, and blood thinners-are cleared from your body by your kidneys. When kidney function declines, these drugs stick around longer. That means higher levels in your blood, which can cause side effects like dizziness, nausea, confusion, or bleeding. In seniors, this isn’t rare. One study found that nearly 1 in 3 hospital admissions for drug toxicity in people over 65 were due to kidney-related dosing errors. The problem isn’t that doctors are careless. It’s that most electronic health records still use outdated formulas to estimate kidney function. Many still default to the old Cockcroft-Gault formula using actual body weight, which overestimates kidney function in thin or frail seniors. Others use CKD-EPI, which works well for middle-aged people but can miss early decline in older adults with low muscle mass. The result? A senior might be told their kidneys are fine, when in reality, they’re barely working.The Four Equations Used to Estimate Kidney Function
There are four main equations doctors use to estimate how well your kidneys are filtering waste. Each has strengths and weaknesses in seniors:- Cockcroft-Gault (CG): This is the oldest formula, developed in 1976. It uses your age, weight, gender, and serum creatinine. The key? It calculates creatinine clearance, which is closer to how drugs are actually removed from your body. But if you use your actual body weight, it overestimates kidney function-especially if you’re overweight or underweight. Using ideal body weight instead improves accuracy by 15-20% in seniors.
- MDRD: Introduced in 1999, this equation estimates glomerular filtration rate (eGFR). It’s widely used but tends to underestimate kidney function in healthy seniors. It doesn’t handle low muscle mass well, which is common in older adults.
- CKD-EPI: Released in 2009, this became the new standard for most clinics. It’s more accurate than MDRD for people with normal or mildly reduced kidney function. But in seniors over 75, especially those who are frail or malnourished, CKD-EPI can miss real kidney decline. One study showed it misclassified nearly 1 in 4 older patients as having better kidney function than they actually did.
- BIS1 and FAS: These are newer equations designed specifically for older adults. BIS1, developed in 2019, uses age, sex, serum creatinine, and serum cystatin C. It’s the most accurate for people over 75. In one study of 85-year-olds, BIS1 was 95% accurate compared to the gold standard, while CKD-EPI was only 78% accurate. FAS is similar and performs just as well.
For seniors, especially those over 75, BIS1 or FAS should be the first choice-not CKD-EPI. But most clinics still use CKD-EPI because it’s pre-set in their software. You have to ask for BIS1.

What to Ask Your Doctor
Don’t assume your kidney function was checked properly. Here’s what to ask at your next appointment:- Which equation did you use to calculate my eGFR? If they say “CKD-EPI” or “MDRD,” ask if they’ve considered BIS1 or FAS, especially if you’re over 75, underweight, or have low muscle mass.
- Did you use my actual weight or ideal body weight? If you’re thin or frail, actual weight can make your kidneys look better than they are. Ideal body weight gives a clearer picture.
- Have you checked my serum cystatin C? This is a newer blood test that’s not affected by muscle mass. If your creatinine-based eGFR is borderline (45-59 mL/min/1.73 m²) but you feel fine and have no protein in your urine, cystatin C can confirm whether your kidneys are truly declining.
- Is my medication dose adjusted for my kidney function? Even if your eGFR is “normal,” many drugs need lower doses in seniors. Ask specifically about blood thinners (like dabigatran or rivaroxaban), antibiotics (like vancomycin), and pain meds (like tramadol).
One real case from a long-term care facility: An 88-year-old woman was on vancomycin for a skin infection. Her eGFR was 48 mL/min/1.73 m² using CKD-EPI. The dose was set at 1,000 mg every 12 hours. She became confused and trembled. Switching to BIS1 showed her true eGFR was 29. The dose was cut in half-and she recovered within days.
When Lab Results Lie: Low Muscle Mass and False Normalcy
Creatinine, the main marker used in kidney tests, comes from muscle. The more muscle you have, the higher your creatinine. That’s why a muscular 70-year-old might have a “normal” creatinine level, while a frail, thin 80-year-old with the same kidney function has a low creatinine-and looks like their kidneys are working fine. This is the biggest trap in senior kidney testing. A “normal” creatinine doesn’t mean normal kidney function. It just means low muscle mass. That’s why cystatin C is so important. It’s made by all body cells, not just muscle. If your creatinine says your kidneys are okay, but your cystatin C says they’re declining-you’ve got a problem. Cystatin C costs about $50-$75 more than a standard creatinine test. But if you’re on a blood thinner, an antibiotic, or a painkiller with a narrow safety window, that extra cost is worth avoiding a hospital stay.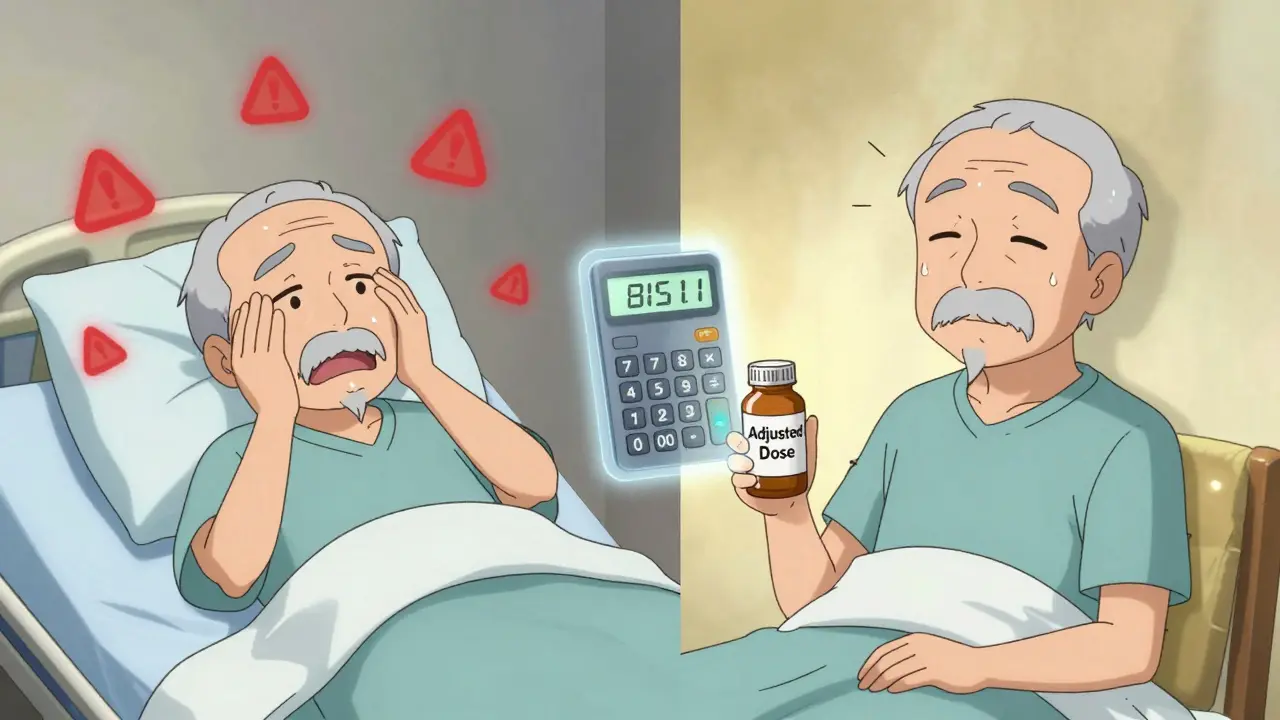
What You Can Do Right Now
You don’t need to wait for your next checkup to protect yourself. Here’s what you can do today:- Know your numbers. Ask for a copy of your last kidney function test. Look for the eGFR number and the equation used. If it’s not listed, ask.
- Keep a medication list. Write down every pill you take, including over-the-counter drugs like ibuprofen or naproxen. Bring it to every appointment.
- Ask for a pharmacist consult. Many hospitals and clinics offer free medication reviews by a clinical pharmacist. They’re trained to spot kidney-related dosing risks.
- Use the National Kidney Foundation’s eGFR calculator. It’s free online and updated for 2024. You can plug in your numbers and see how different equations change your result.
One woman in Perth, 82, started checking her eGFR after her husband had a bad reaction to a blood thinner. She used the NKF calculator and found her CKD-EPI eGFR was 58, but BIS1 showed 41. She told her doctor, and they switched her to a safer dose. She’s been fine for 18 months.
The Future: AI, Personalized Dosing, and Better Tools
The medical world is starting to wake up. In 2024, a new equation called CKD2024 was introduced-it combines creatinine and cystatin C with age-specific adjustments. Early results show it’s 15% more accurate for people over 80. The National Institute on Aging is funding a $4.2 million project to build point-of-care kidney tests that account for muscle loss and frailty. Some hospitals are already using AI tools that look at your age, weight, muscle mass, nutrition, and other health conditions to recommend the best equation for you. In a 2023 pilot at Mayo Clinic, these tools cut dosing errors by 22%. But until these tools are everywhere, the power is still in your hands. You’re not just a patient. You’re the most important person in your own care.What’s the best way to check kidney function in seniors?
For seniors over 75, the BIS1 or FAS equation is the most accurate. These were designed specifically for older adults and handle low muscle mass better than older formulas like CKD-EPI or MDRD. If your doctor only uses CKD-EPI, ask for BIS1. Adding a serum cystatin C test can confirm results if your creatinine looks normal but you’re frail or thin.
Why does my doctor keep using CKD-EPI if it’s not accurate for seniors?
Most electronic health records automatically use CKD-EPI because it became the national standard in 2012. Doctors often don’t realize it’s less accurate for older adults with low muscle mass. It’s not that they’re wrong-they’re using what the system defaults to. You have to ask for BIS1 or FAS. Some hospitals, like the University of Michigan, now auto-select BIS1 for patients over 75.
Can I trust my creatinine level if it’s normal?
Not always. Creatinine comes from muscle. If you’ve lost muscle due to aging, illness, or poor nutrition, your creatinine can be low-even if your kidneys aren’t working well. That’s why a normal creatinine doesn’t mean normal kidney function. Always ask for the eGFR calculation and the equation used. If you’re thin or frail, request a cystatin C test.
Which medications are most dangerous if kidney function is off?
Blood thinners like dabigatran and rivaroxaban, antibiotics like vancomycin and aminoglycosides, painkillers like tramadol and morphine, and diabetes drugs like metformin are high-risk. Even common NSAIDs like ibuprofen can cause kidney damage in seniors with reduced function. Always check if your medication dose is adjusted for kidney function.
How often should seniors get their kidney function checked?
At least once a year if you’re over 70. If you have diabetes, high blood pressure, or take multiple medications, check every 6 months. If you’re hospitalized or start a new high-risk medication, get tested before and after. Don’t wait for symptoms-by then, it’s often too late.


Kathy McDaniel
January 26, 2026 AT 23:59OMG this is so real 😭 I just got back from my grandma's doc visit and she's on rivaroxaban and they used CKD-EPI... she's 84, weighs 98 lbs, and they said her kidneys are 'fine'. I had to pull up BIS1 on my phone right there. She's been fine since they lowered her dose. Please, everyone, ask for BIS1. It's not that hard.
Kirstin Santiago
January 28, 2026 AT 17:43I'm a geriatric nurse and I see this every week. Doctors rely on the EHR defaults like it's gospel. But if you're thin, frail, or over 75? That 'normal' creatinine is a lie. I always push for cystatin C when the numbers don't match how the patient feels. It's not expensive, and it saves lives. Just ask.
Desaundrea Morton-Pusey
January 29, 2026 AT 17:22Of course this is a problem. The medical system is broken. They still use 1970s tech to treat 2024 humans. I swear, if I had a dollar for every time a senior got poisoned by a 'normal' lab result... I'd buy a private island. Also, why is this even a thing? Shouldn't this be automatic?
Harry Henderson
January 30, 2026 AT 17:21STOP WAITING FOR DOCTORS TO SAVE YOU. You're the only one who cares enough to read this. Print this out. Take it to your appointment. Highlight the BIS1 part. If they roll their eyes? Find a new doctor. Your life isn't a lab experiment. Take control. Now.
suhail ahmed
February 1, 2026 AT 15:34Bro, this is the kind of knowledge that should be taught in med schools, not buried in journals. In India, we don't even have cystatin C in most clinics, but I tell my elderly patients: if you're skinny and your creatinine looks 'good' but you're tired all the time? You're being gaslit by your own kidneys. Ask. Demand. Be annoying. It's worth it.
Anjula Jyala
February 2, 2026 AT 10:10CKD-EPI is standard because it's validated in large cohorts. BIS1 has limited external validation. You're cherry-picking outliers. Also, cystatin C is expensive and not cost-effective for population screening. Stop overmedicalizing aging. Kidney function declines naturally. Don't turn every 80-year-old into a patient needing 5 tests.
Paul Taylor
February 4, 2026 AT 10:04I've been managing my dad's meds since he turned 78 and let me tell you this is the most important thing I've ever learned. We used to think his creatinine was normal so we didn't worry. Then he started getting confused after antibiotics. We switched to BIS1 and his eGFR dropped from 52 to 31. They halved his dose and he's been like a new man. Don't assume. Don't trust. Ask. Ask. Ask. And write it down. Keep a notebook. I have three pages of meds and eGFRs. It saved his life.
Kegan Powell
February 4, 2026 AT 20:29we're all just trying to survive the system 💙 the fact that you have to fight just to get your kidneys measured right... it's insane. but you're not alone. i'm 62 and now i check my own eGFR with the NKF calculator before every visit. my doc thinks i'm obsessive. i think i'm smart. if your body's changing and the tools haven't caught up? you gotta be the bridge. and hey... if you're reading this, you already are 🙌
April Williams
February 6, 2026 AT 12:14Why are we letting doctors get away with this? This is malpractice. They're using outdated formulas on elderly people and calling it standard care? That's not negligence, that's criminal. Someone should sue every hospital that doesn't auto-switch to BIS1 for patients over 75. This isn't about being 'proactive'-it's about basic human dignity.
Candice Hartley
February 7, 2026 AT 17:22My mom’s cystatin C came back high even though her creatinine was normal. She’s 81, thin, and had zero symptoms. They lowered her tramadol dose and she stopped falling. Just ask for it. It’s one blood test. 💕