Starting a new medication can feel like stepping into the unknown. You’re hoping for relief - better blood pressure, clearer mood, fewer headaches - but then comes the nausea, the dry mouth, the fatigue. It’s common. In fact, mild side effects happen to 50-70% of people when they begin a new drug, according to a 2023 review in the Journal of Clinical Pharmacy and Therapeutics. The good news? Most of these aren’t dangerous. And you don’t have to quit the medication to feel better.
What Counts as a Mild Side Effect?
Not every weird feeling means something’s wrong. Mild side effects are temporary, low-intensity reactions that usually show up in the first week or two. They’re your body adjusting. Common ones include:- Nausea or an upset stomach
- Diarrhea or constipation
- Dry mouth
- Mild fatigue or drowsiness
- Headache
- Light dizziness
How to Handle Nausea and Upset Stomach
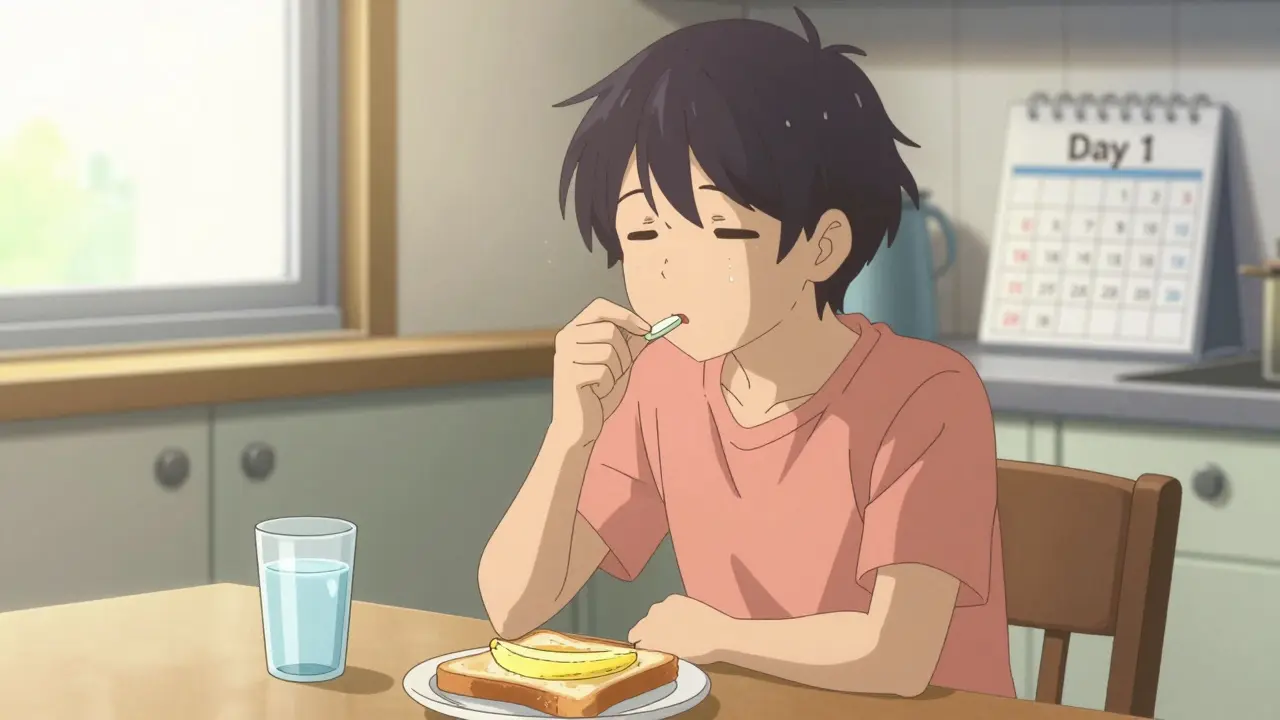
Nausea is the #1 reason people stop taking meds. But it’s often easy to fix. Here’s what works:- Take it with food - not on an empty stomach. For 78% of non-antibiotic drugs, eating a light snack or meal with the pill cuts nausea by half. A 2022 Mayo Clinic study showed 62% of people felt better within 72 hours just by doing this.
- Avoid spicy, greasy, or acidic foods - they irritate your stomach more. Stick to bland options like toast, rice, or bananas.
- Drink 8-10 ounces of water right after taking the pill. It helps the medicine move through your system faster and reduces stomach irritation.
- Don’t lie down for at least 30 minutes after taking it. Gravity helps keep things where they belong.
Managing Diarrhea and Constipation
Digestive changes are common with antibiotics, antidepressants, and pain meds. But you don’t have to suffer.For diarrhea:
- Avoid caffeine (coffee, soda, energy drinks) - it speeds things up.
- Stay away from acidic foods like citrus, tomatoes, or vinegar (anything with pH under 4.5).
- Limit high-fiber foods to under 25g per day for a few days. That means less beans, bran, and raw veggies.
- Try loperamide (Imodium) - but only after checking with your pharmacist. Studies show it works in 73% of cases when used correctly.
For constipation:
- Drink 2.5-3 liters of water daily. That’s about 10-12 glasses. Dehydration makes constipation worse.
- Add 30-35g of fiber daily - think apples, pears, broccoli, oats. A 2021 trial with over 1,200 people showed 68% of symptoms improved with this combo.
- Move your body. Even a 30-minute walk each day helps your gut get moving.
Dealing with Dry Mouth
Dry mouth isn’t just annoying - it can lead to cavities, sore gums, and trouble swallowing. But it’s easy to fix.- Sip water every 15-20 minutes. Keep a bottle nearby. Don’t wait until you’re thirsty.
- Suck on sugar-free sour candies - the kind with citric acid. They stimulate saliva. A 2022 study in the Journal of the American Dental Association found 79% of users saw improvement within 48 hours.
- Use xylitol gum or sprays. Xylitol doesn’t just help saliva - it fights cavity-causing bacteria.
- Avoid alcohol-based mouthwashes. They dry you out more.
Many people say the sour candy trick was a game-changer. One Amazon review of XyliMelts (a popular product) had 1,850 ratings and a 4.7-star average. People didn’t just tolerate it - they loved it.

Beating Fatigue and Low Energy
Feeling wiped out on a new med? You’re not lazy. Your body’s working hard to adjust.- Eat balanced meals: 45-65% carbs, 20-35% fats, 10-35% protein. Skipping meals makes fatigue worse.
- Get 150 minutes of moderate exercise per week - that’s 30 minutes, 5 days a week. Walking, cycling, even gardening counts.
- Sleep 7-9 hours every night. Even one night of poor sleep can undo progress.
A 2021 NIH study (NCT04321987) tracked over 800 people on meds that caused fatigue. Those who followed this routine saw a 63% improvement in energy within two weeks. It’s not magic - it’s biology.
The Mindset Trick That Changes Everything
Here’s something you won’t hear from every doctor: your side effects might mean the drug is working.Harvard researchers led by Dr. Alia Crum ran three trials starting in 2018. They gave one group standard advice: “These side effects are annoying, but they’ll pass.” The other group was told: “These sensations show your body is responding to the treatment.”
The results? The second group reported 40% less symptom intensity and 35% fewer calls to their doctor. It worked best for meds with high placebo responses - like antidepressants (SSRIs) and blood pressure drugs. Why? Because your brain plays a big role in how you feel.
This doesn’t mean ignore real danger. But for mild, temporary reactions? Reframing them as signs of progress can reduce anxiety and help you stick with the treatment.
What NOT to Do
Some things seem helpful - but aren’t.- Don’t stop without talking to your provider. You might be giving up on something that could work.
- Don’t double up on OTC meds. Taking extra antacids, laxatives, or sleep aids without checking can cause dangerous interactions.
- Don’t assume all side effects are normal. Shortness of breath, chest pain, swelling, or rash? Call your doctor right away. Dr. Michael Stebbins of UCSF warns that 12% of hospital admissions from medication issues come from people mistaking serious symptoms for “normal side effects.”

When to Call Your Doctor or Pharmacist
You don’t need to panic. But you do need to know when to speak up.Wait 72 hours before calling - unless symptoms are severe. Why? Many mild side effects fade on their own. A 2022 Rx Outreach program found that waiting 3 days cut unnecessary calls by 45%.
When you do call, be specific:
- “I’ve had nausea every morning since Monday.”
- “I’ve tried taking it with food and water, but it hasn’t helped.”
- “I’m also taking [other meds] - could they be interacting?”
Pharmacists are your best allies here. In 2023, 52% of initial side effect questions were handled by community pharmacists - not doctors. They’re trained to help you stay on track.
Why This Matters - Beyond Comfort
Stopping a medication because of mild side effects isn’t just inconvenient - it’s costly. A 2023 IQVIA analysis found that patients who stick with their treatment thanks to proper side effect management save $1,200-$1,800 a year in avoided ER visits and hospital stays.And it’s not just money. People who manage side effects well have 65-80% higher adherence rates at the 6-month mark. That means better control of diabetes, lower stroke risk, fewer depression relapses, and more stable blood pressure.
Health systems are catching on. UnitedHealthcare reported a 22% drop in medication discontinuations after launching their “Side Effect Navigator” program. The FDA is now requiring all new drug labels to include clear, actionable side effect tips. By 2026, this will be standard.
Final Tip: Be Specific With Instructions
Generic advice like “take with food” doesn’t work. People forget. A Harvard Health study showed that when patients got exact instructions - “take with 8 ounces of milk at 8 a.m.” - adherence jumped from 41% to 73%.So if your doctor says “take it with food,” ask: “What kind of food? Should I take it before or after? What time?” The more specific, the better.
Can I stop my medication if the side effects are too uncomfortable?
It’s usually safer to manage the side effect than to stop. Most mild side effects fade within 1-2 weeks. Stopping abruptly can cause withdrawal symptoms or make your original condition worse. Always talk to your doctor or pharmacist first - they can suggest adjustments like timing, dosage, or diet changes that help you stay on track.
Are there side effects I should never ignore?
Yes. If you experience chest pain, shortness of breath, swelling in your face or throat, severe rash, confusion, or irregular heartbeat - call emergency services or go to the ER. These aren’t mild side effects. They’re warning signs. Even if you’ve been told “this is normal,” trust your body. It’s better to be safe than sorry.
How long should I wait before deciding the side effects won’t go away?
Give it 7-14 days. Most mild side effects peak in the first 3-5 days and then fade. If they’re still bothering you after two weeks, it’s time to talk to your provider. But don’t assume it’s the medication - sometimes it’s timing, diet, or another drug interacting with it.
Can my pharmacist help with side effects?
Absolutely. Pharmacists are trained to help you manage side effects. They know which drugs interact with food, which ones cause dry mouth, and what OTC options are safe. In fact, over half of all side effect questions are first addressed by pharmacists. Don’t hesitate to walk in or call - they’re there to help you stay on your medication.
Why do some people have side effects and others don’t?
It’s a mix of genetics, age, diet, other medications, and even your mindset. A 2023 NIH study found that AI tools can now predict side effect risk with 68% accuracy based on your DNA, weight, and current meds. But even with the same drug, two people can react completely differently. That’s why personalized advice - not one-size-fits-all - is the future of medication management.