Fentanyl Patch Heat Exposure Calculator
Critical Safety Reminders
- Never apply direct heat to the patch area
- Avoid hot baths, saunas, and tanning
- Use lukewarm water (below 105°F)
- Never leave heating pads on for extended periods
- Dispose of used patches safely
Risk Assessment
Enter your details to see risk level...
It sounds impossible - a patch on your skin, meant to ease pain, could kill you if you get too warm. But for people using fentanyl patches, this isn’t a myth. It’s a documented, deadly risk. Fentanyl patches deliver a powerful opioid slowly through the skin. They’re designed for chronic pain in patients who already take opioids regularly. But when heat gets involved - a heating pad, a hot shower, even a fever - the patch can release too much fentanyl, too fast. And that can stop your breathing.
How Fentanyl Patches Are Supposed to Work
Fentanyl patches, like Duragesic, are made to release a steady dose of the drug over three days. The patch doesn’t just drip fentanyl onto your skin. It holds the drug in a special gel layer, and the skin slowly pulls it into your bloodstream. This process takes time. It can take up to 72 hours to reach the full pain-relieving level. That’s why doctors only prescribe them for people who are already used to strong opioids. For someone who’s never taken opioids before, even one patch can be fatal.The system works because the skin acts like a gate. It controls how much fentanyl enters the body. But that gate isn’t foolproof. Heat changes everything.
Why Heat Is So Dangerous
When your skin gets warm, your blood vessels expand. More blood flows to the surface. That sounds harmless - until you’re wearing a fentanyl patch. Suddenly, the drug isn’t being absorbed slowly. It’s being sucked into your bloodstream like a sponge soaking up water.Studies show that raising skin temperature to just 40°C (104°F) can boost fentanyl levels in your blood by 33%. That’s not a small increase. That’s enough to push someone into overdose territory. In one experiment, researchers used a special heat pad over a fentanyl patch. Within hours, blood levels of fentanyl tripled. The volunteers didn’t feel sick at first. But their breathing slowed dangerously.
This isn’t just lab data. Real patients have died. There are documented cases where people overdosed after:
- Using a heating pad for back pain
- Being wrapped in a warming blanket during surgery
- Doing heavy exercise that raised their body temperature
Even something as simple as a hot bath or sunbathing can be risky. The patch doesn’t care if the heat is intentional or accidental. It reacts the same way.
What Counts as Heat? (It’s More Than You Think)
Most people know not to use a heating pad. But the dangers go deeper.- Hot showers or baths - Water over 105°F can heat your skin enough to change absorption.
- Saunas and steam rooms - These environments raise core body temperature. Even 15 minutes can be dangerous.
- Electric blankets - Left on all night, they keep the patch warm for hours.
- Tanning lamps and sunlamps - These aren’t just for tanning. They’re heat sources.
- Fever - A temperature of 101°F or higher can increase fentanyl absorption. Doctors tell patients to call immediately if they get sick.
- Physical exertion - Lifting heavy objects, walking fast in hot weather, even shoveling snow - all can raise body heat.
- Hot environments - Working outside in summer, sitting near a radiator, or even driving in a hot car with the heater on.
One study found that patients wearing fentanyl patches during dental procedures were at high risk. Why? Sedation drugs can dilate blood vessels. Combined with the patch, that’s a recipe for overdose.
What Happens After You Remove the Patch?
Many people think once they peel off the patch, the danger is over. It’s not.Even after removal, the patch still holds enough fentanyl to keep releasing the drug for hours - sometimes up to 24 hours. If you take a hot shower right after taking off the patch, or wrap yourself in a blanket, you’re still at risk. The drug is still in your skin, still being absorbed. You can overdose even after the patch is gone.

Who Should Never Use Fentanyl Patches?
Fentanyl patches are not for everyone. They are contraindicated for:- People who have never taken opioids before (opioid-naïve)
- Patients with acute pain, like after surgery
- People with breathing problems, like sleep apnea
- Anyone allergic to fentanyl or the patch materials
They’re meant for cancer patients or those with severe, long-term pain who’ve already built up tolerance to other opioids. Even then, they’re only prescribed after careful evaluation. If you’re new to opioids, even a low-dose patch can kill you.
Other Medications That Make It Worse
Fentanyl is broken down in your liver by enzymes called CYP3A4. Some common drugs block these enzymes. That means fentanyl stays in your body longer - and builds up to dangerous levels.Drugs that can cause this dangerous interaction include:
- Ketoconazole (an antifungal)
- Erythromycin (an antibiotic)
- Clarithromycin (another antibiotic)
- Some HIV medications
- Some antidepressants
If you’re on any of these, tell your doctor before using a fentanyl patch. The combination can lead to sudden, life-threatening overdose - even without heat exposure.
Signs You’re Overdosing
Overdose doesn’t always come with screaming or collapse. Sometimes, it’s quiet. Here’s what to watch for:- Slow, shallow, or stopped breathing
- Extreme drowsiness - you can’t stay awake
- Confusion or dizziness
- Cold, clammy skin
- Blue lips or fingernails
- Unresponsiveness
Also watch for signs of serotonin syndrome - a rare but dangerous reaction:
- Rapid heartbeat
- High fever
- Muscle spasms or stiffness
- Agitation or hallucinations
If you see any of these, call emergency services immediately. Naloxone (Narcan) can reverse opioid overdose, but it must be given fast.
What to Do If You Use Fentanyl Patches
If you or someone you care for uses these patches, follow these rules:- Never apply heat - no heating pads, hot tubs, saunas, or electric blankets.
- Avoid prolonged sun exposure. Don’t sunbathe.
- Take lukewarm showers, not hot ones.
- Don’t exercise intensely. Walk gently. Avoid heavy lifting.
- If you get a fever, call your doctor. Don’t wait.
- Remove the patch exactly after 72 hours. Don’t leave it on longer.
- Dispose of used patches safely - fold them in half with the sticky sides together and throw them in the trash where kids or pets can’t reach them.
- Tell every doctor, dentist, or nurse you see that you’re using a fentanyl patch.
- Keep naloxone on hand if you live alone or care for someone at risk.
Why This Risk Is Still Out There
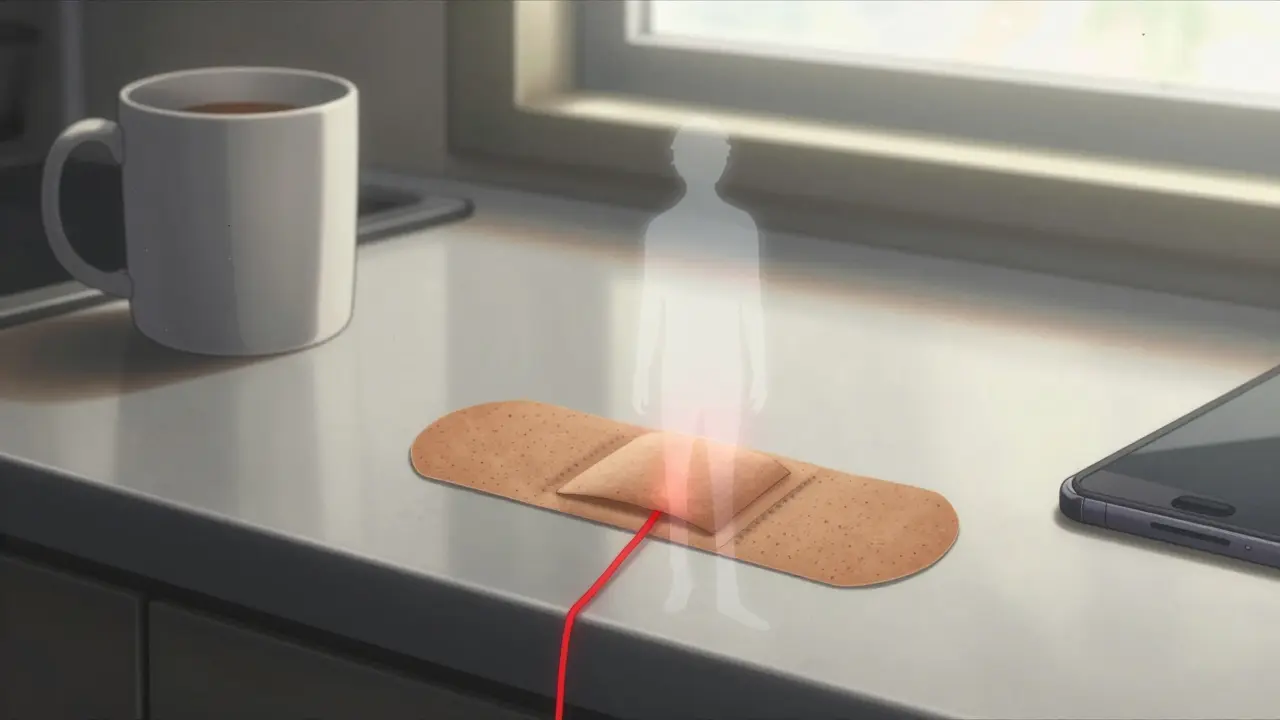
Despite years of warnings, people still get hurt. Why? Because the risk isn’t obvious. A patch looks like a Band-Aid. Heat feels normal. A hot shower after a long day? It’s relaxing. But for someone on fentanyl, it’s a gamble with their life.Doctors don’t always explain the risks clearly. Patients forget. Family members don’t know. And by the time someone realizes something’s wrong, it’s too late.
Regulators like the FDA and health agencies have issued warnings. Hospitals have protocols. But the real protection comes from education - not just once, but over and over.
The Bottom Line
Fentanyl patches can help people live with chronic pain. But they’re not safe unless used with extreme care. Heat isn’t just a caution - it’s a red flag. One wrong move - a hot bath, a fever, a blanket left on too long - can turn a pain treatment into a death sentence.If you’re using one, treat it like a loaded gun. Respect the rules. Talk to your doctor. Know the signs. And never, ever let heat touch that patch.


Aboobakar Muhammedali
December 19, 2025 AT 12:43My uncle used one of these after his back surgery and didn't know about the heat thing. He took a hot shower after removing the patch and passed out in the bathroom. We found him blue. Naloxone saved him but he's been scared of water ever since. Don't play with this stuff.
Kevin Motta Top
December 20, 2025 AT 09:19My dad's on these for cancer pain. We keep the house at 70, no blankets on the patch area, and he showers with lukewarm water. It's not hard. Just respect the damn patch like it's a live wire.
Erica Vest
December 21, 2025 AT 00:44According to FDA guidance, fentanyl patches should never be used in opioid-naive patients, and heat exposure increases bioavailability by up to 33%. The risk is well-documented in peer-reviewed literature since 2005. Always consult a pharmacist before combining with CYP3A4 inhibitors.
Kinnaird Lynsey
December 22, 2025 AT 23:37Wow. So now we're blaming the patch for people who can't follow basic instructions? I guess we should put warning labels on forks too because someone once choked on spaghetti.
Laura Hamill
December 24, 2025 AT 15:10THEY KNOW THIS. THE PHARMA COMPANIES KNOW THIS. THEY DON'T CARE. THEY MAKE BILLIONS. THEY PUT THESE ON THE MARKET LIKE THEY'RE BAND-AIDS. AND NOW PEOPLE ARE DYING. THIS ISN'T AN ACCIDENT. IT'S A COVER-UP. 🤬
Edington Renwick
December 26, 2025 AT 06:46Look, I get it. You're scared. But this isn't about fearmongering. It's about education. My sister's a nurse. She says 80% of the patients on these patches have no idea about the heat risk. Even their doctors forget to mention it. It's not the patch's fault. It's the system's failure.
My cousin died because his wife put a heating pad on his back for "arthritis" - he had a fentanyl patch under it. She didn't know. No one told her. That's the tragedy. Not the patch. Not the heat. The silence.
People think opioids are just for addicts. But this? This is for grandma with terminal cancer who just wants to sleep without screaming. And now she's dead because someone didn't say "don't take a hot bath."
Stop blaming the victim. Start blaming the silence.
benchidelle rivera
December 26, 2025 AT 21:06As a palliative care nurse for 18 years, I've seen too many preventable deaths. This post is accurate. Every single point. But here's what no one says: hospitals don't train staff on this. Families aren't given printed handouts. Pharmacies don't call patients back to confirm understanding. We're relying on patients to read a tiny warning label on a patch that looks like a Band-Aid. That's not safety. That's negligence.
If you're using one, print this post. Tape it to the mirror. Show your family. Tell every doctor you see. And if you're not sure - don't use it. There are safer options. This isn't worth your life.
Alisa Silvia Bila
December 27, 2025 AT 11:58Thank you for this. My mom is on one. I didn't know about the post-removal risk. We're changing everything today.