Gabapentinoid-Opioid Risk Assessment Tool
This tool assesses your risk of respiratory depression when taking gabapentinoids (gabapentin, pregabalin) with opioids. It's designed to help you understand your potential risk factors and have informed conversations with your healthcare provider.
Your Risk Assessment
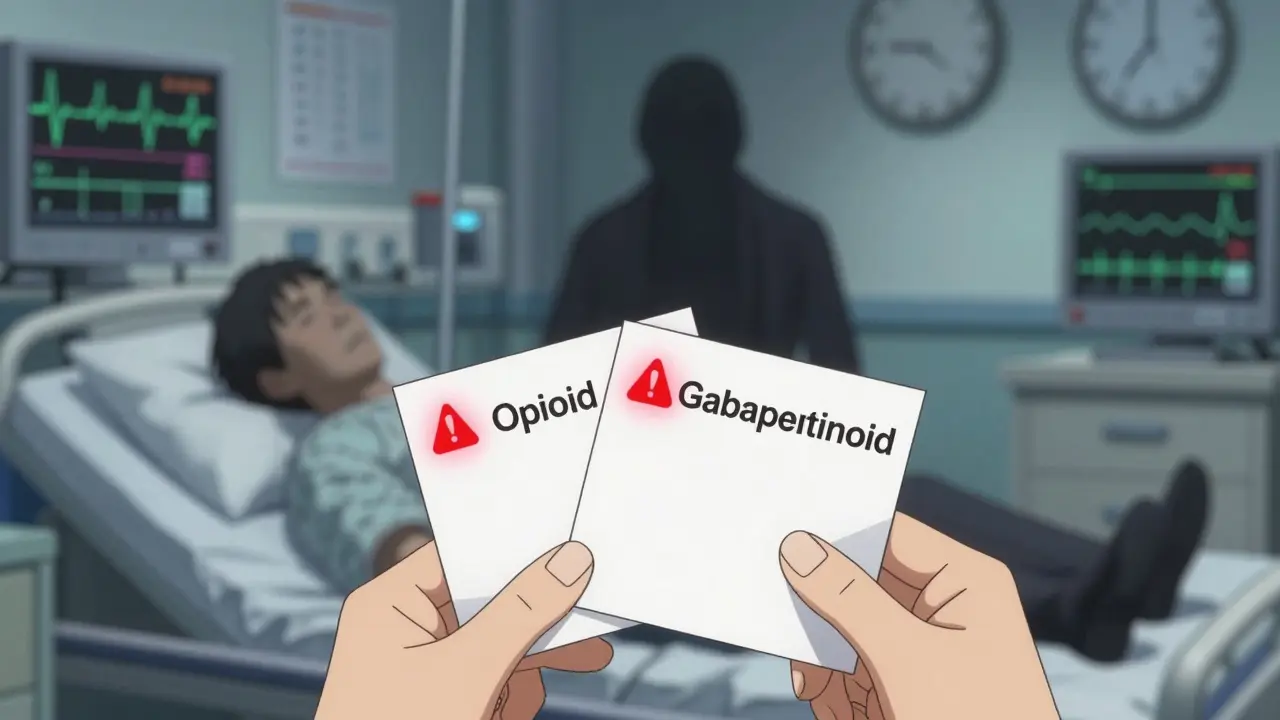
The Silent Risk No One Talks About
When you take gabapentin or pregabalin for nerve pain, and your doctor adds an opioid like oxycodone or hydrocodone for extra relief, you might think you’re getting better control. But what you’re not being told is that this combination can slow your breathing to a dangerous level - even if you’ve taken both drugs before without issue. This isn’t a rare side effect. It’s a life-threatening interaction that’s been documented in thousands of cases, and it’s still happening every day.
How Gabapentinoids Alone Can Slow Your Breathing
Gabapentin and pregabalin aren’t just harmless nerve calmers. They act on the central nervous system - the same area that controls breathing. Studies show that even on their own, these drugs can cause respiratory depression. One trial with healthy volunteers found that a single dose of gabapentin led to significantly more pauses in breathing during sleep compared to placebo. Another study showed that end-tidal CO2 levels - a direct measure of how well you’re exhaling - rose when people took pregabalin alone. This means your body isn’t clearing carbon dioxide the way it should. And if you already have lung disease, sleep apnea, or are over 65, your risk jumps dramatically.
Why Combining Them With Opioids Is a Recipe for Disaster
The real danger kicks in when gabapentinoids are mixed with opioids. Both types of drugs depress the brainstem - the part that tells your lungs to breathe. When you combine them, the effect isn’t just added. It’s multiplied. The FDA reviewed over 100 cases of respiratory depression linked to gabapentinoids. Ninety-two percent involved either another CNS depressant (like opioids) or an existing breathing problem. Twenty-four percent of those cases ended in death. Every single fatal case had at least one risk factor: age, kidney issues, lung disease, or another sedative.
It gets worse. A major 2017 study of over 16 years of patient data found that people taking both gabapentin and an opioid were 50% more likely to die from an opioid-related cause. Those on very high doses of gabapentin? Their risk nearly doubled. This isn’t theoretical. This is happening in real clinics, in real homes, to real people.
Why Doctors Keep Prescribing Both - And Why It’s Dangerous
Back in 2016, the CDC pushed doctors to reduce opioid prescriptions. Many turned to gabapentinoids as a "safer" alternative for pain. But here’s the catch: gabapentinoids don’t make opioids safer. They make them deadlier. In 2017, nearly one in four new gabapentin prescriptions came with an opioid. That’s not coincidence. It’s a dangerous trend that’s still going strong, despite warnings from the FDA and UK’s MHRA in 2019.
Worse still, the evidence that gabapentinoids actually improve pain control when paired with opioids is weak. One large study of over 5.5 million surgical patients found no clear benefit in pain relief from combining the two. The main reason they’re prescribed together? Habit - not science. And the cost? Lives.
Who’s Most at Risk - And What to Watch For
You’re at higher risk if you:
- Are over 65
- Have chronic lung disease (COPD, asthma, sleep apnea)
- Have kidney problems - gabapentin and pregabalin are cleared by the kidneys, and poor function means higher drug levels
- Take other sedatives like benzodiazepines or alcohol
- Are taking high doses of either drug
Signs to watch for: unusual drowsiness, confusion, slow or shallow breathing, bluish lips or fingertips, difficulty waking up. If you or someone you care for is on both drugs and shows any of these signs, seek help immediately. Don’t wait. Respiratory depression can turn fatal in minutes.

What You Should Do - Practical Steps to Stay Safe
If you’re currently taking gabapentin or pregabalin with an opioid:
- Don’t stop either drug suddenly. That can cause seizures or withdrawal.
- Ask your doctor to review your dose. The FDA and Medical Letter both recommend starting low and going slow - especially if you’re older or have kidney issues.
- Ask: "Is this combination really necessary?" There’s little proof it improves pain, but plenty of proof it increases death risk.
- Get your kidney function checked. If your creatinine clearance is below 60 mL/min, your gabapentinoid dose likely needs adjustment.
- Keep naloxone on hand if you’re on opioids. It won’t reverse gabapentinoid effects, but it can help if opioids are the main driver of breathing trouble.
For chronic pain, consider alternatives with less risk: physical therapy, cognitive behavioral therapy, or non-opioid medications like duloxetine or topical lidocaine. They may not work as fast, but they won’t stop your breathing.
The Bottom Line
Gabapentinoids aren’t harmless. Opioids aren’t safe. Together, they’re a lethal mix. The science is clear. The warnings are out. Yet this deadly combination is still being prescribed daily. You don’t need both. You don’t benefit much from the combo. But you could die from it. If you’re on either of these drugs, talk to your doctor - not tomorrow, not next week. Today. Ask if you really need both. And if the answer isn’t a clear, evidence-based yes, push for a safer plan.
Why This Isn’t Just a "Prescription Problem"
This isn’t just about doctors prescribing too much. It’s about a system that treats pain like a math problem - add more drugs, get more relief. But the body doesn’t work that way. Sometimes, adding more drugs doesn’t fix the problem. It creates a new, deadlier one. The rise in gabapentinoid use was meant to reduce opioid harm. Instead, it created a hidden epidemic of respiratory depression. We need better tools, better guidelines, and better conversations. But until then, the most powerful thing you have is your voice. Ask questions. Demand answers. Protect your breathing.


Harbans Singh
December 25, 2025 AT 10:29Michael Dillon
December 25, 2025 AT 22:04Lindsay Hensel
December 26, 2025 AT 03:00Gary Hartung
December 26, 2025 AT 23:52Oluwatosin Ayodele
December 27, 2025 AT 02:54Jason Jasper
December 28, 2025 AT 22:25Mussin Machhour
December 29, 2025 AT 07:11Carlos Narvaez
December 30, 2025 AT 23:03Winni Victor
January 1, 2026 AT 10:34Sophie Stallkind
January 3, 2026 AT 04:48Katherine Blumhardt
January 4, 2026 AT 07:27Bailey Adkison
January 6, 2026 AT 04:42Ben Harris
January 7, 2026 AT 22:29Justin James
January 8, 2026 AT 08:40Zabihullah Saleh
January 8, 2026 AT 19:46