Beta-Blocker Exercise Intensity Calculator
How Intense Are You Exercising?
Beta-blockers affect heart rate response. Use these proven methods instead of heart rate monitors.
Intensity Result
Why This Matters
Beta-blockers artificially limit your heart rate response. Your body's perception of effort is now the most reliable indicator of safe exercise intensity.
When you're on beta-blockers for high blood pressure, heart disease, or irregular heartbeat, your body doesn't respond to exercise the way it used to. You might find yourself getting winded faster, feeling more tired than usual, or noticing you can't push as hard during a walk or bike ride. This isn't just in your head-it's a direct effect of the medication. Beta-blockers like metoprolol, propranolol, and atenolol work by slowing your heart rate and reducing the force of your heartbeat. That's great for your heart, but it also means your body can't pump as much blood to your muscles when you're active. The result? Fatigue. And if you keep pushing yourself the same way you did before, you risk overexertion or even injury.
Why Beta-Blockers Make You Feel Tired During Exercise
Beta-blockers block adrenaline, the hormone that tells your heart to race during physical activity. Normally, your heart rate might jump from 70 bpm at rest to 160+ bpm during a hard run. On beta-blockers, that same run might only raise your heart rate to 120-130 bpm. This isn't a sign you're getting weaker-it's a sign the drug is working. But here's the catch: your muscles need oxygen, and oxygen is delivered by blood flow. Less heart rate means less blood flow. Studies show that beta-blockers can cut your VO₂ max (your body's maximum oxygen use during exercise) by 10-15%. That's like losing the fitness of several months of training overnight.
It's not just about heart rate. Your blood pressure response changes too. On regular days, your systolic pressure (the top number) might climb 30-50 mmHg during a workout. On beta-blockers, it might only go up 10-20 mmHg. Your body tries to make up for it by pulling more oxygen out of the blood and using more stored energy-but that doesn't always work. Many people report feeling exhausted even during light activity. Some even notice dry mouth or not sweating at all during exercise-a red flag for dehydration that needs immediate attention.
How Other Heart Medications Compare
Not all heart meds affect exercise the same way. ACE inhibitors like lisinopril or calcium channel blockers like amlodipine don't slow your heart rate like beta-blockers do. They might cause leg swelling or dizziness, but they don't limit your heart's ability to speed up. Diuretics can mess with your electrolytes and cause cramps, but again, they don't directly cap your heart rate. That makes beta-blockers unique-and more challenging for active people. If you're on multiple medications, it's important to know which one is likely causing your fatigue. Beta-blockers are the main culprit when it comes to exercise performance drops.
Forget Heart Rate Monitors-Use These Instead
Here's the biggest mistake people make: trying to hit a target heart rate while on beta-blockers. If your old target was 130 bpm, and you're now only hitting 110, you might think you're not working hard enough. But that's not true. Your heart rate is being artificially held back. Trying to push it higher can lead to dangerous overexertion. Instead, use these three proven alternatives:
- The Talk Test: If you can talk comfortably but not sing, you're at the right intensity. This is the simplest, most reliable method endorsed by the American Heart Association. No gadgets needed.
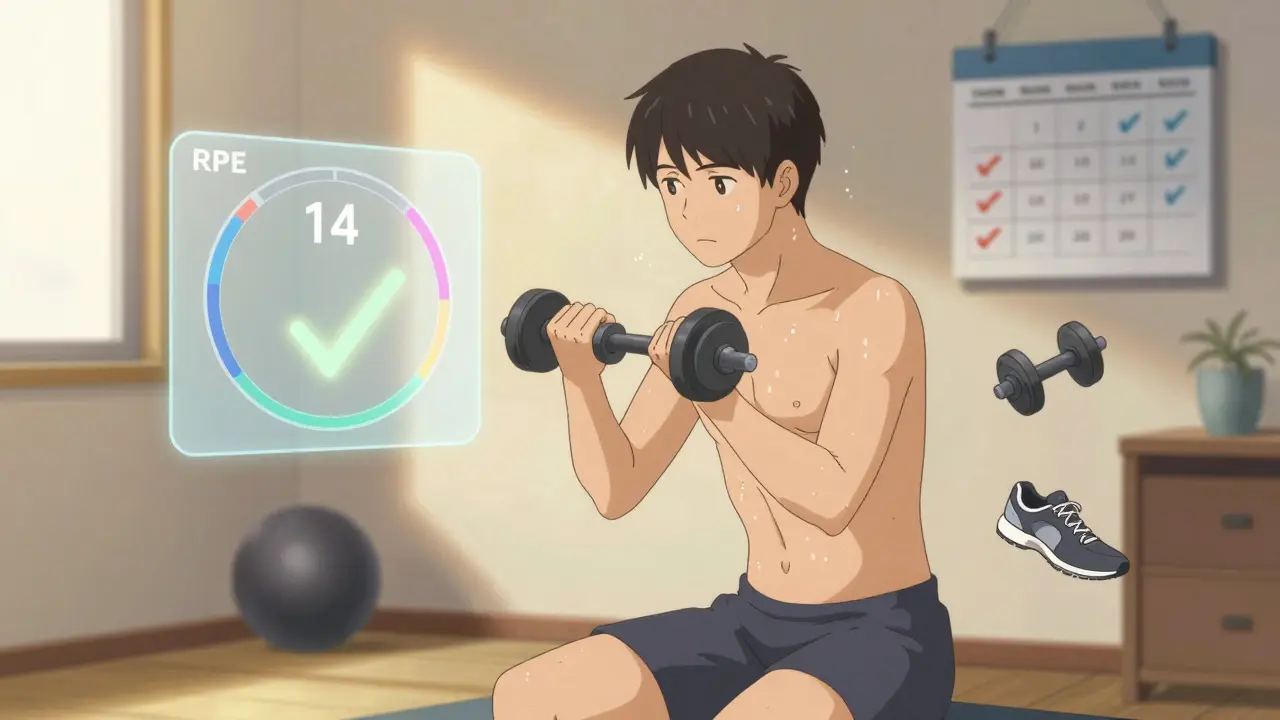
- The Borg RPE Scale: This is a 6-20 scale where 6 means no effort and 20 means maximum effort. On beta-blockers, aim for 12-14 for moderate exercise (like brisk walking) and 15-17 for vigorous (like uphill hiking). Most people find they need to drop their target by one level. If you used to aim for 16, now aim for 14.
- Perceived Effort: Ask yourself: "How hard am I working right now?" If you feel like you're working moderately, you probably are-even if your watch says otherwise.
One user on the American Heart Association's support forum shared: "Switching from heart rate tracking to the talk test let me safely maintain my walking routine on 50mg atenolol." That’s the kind of change that makes a real difference.
How to Adjust Your Workout Routine
Don’t quit exercising. Just change how you do it.
- Extend your warm-up: Instead of 5-10 minutes, spend 10-15 minutes easing into activity. This gives your heart time to adjust gradually. A slow walk or light cycling works well.
- Lengthen your sessions: Since each minute of exercise is less intense, you need more minutes to get the same benefit. Aim for 180-188 minutes of moderate activity per week instead of the standard 150. Break it into 30-40 minute sessions, five days a week.
- Reduce intensity, not frequency: Swap high-intensity intervals for steady, longer walks or rides. If you used to do sprint intervals, try walking on an incline instead. You’ll still build endurance without overloading your heart.
- Adjust strength training: Beta-blockers don’t weaken your muscles-they just limit your heart’s ability to support them. So reduce your weights by 15-20%, but keep the same number of reps. You’ll still build strength safely.
Research from Dr. Sheldon E. Litwin at Oregon Health & Science University found that interval training with a 2:1 work-to-rest ratio (like 4 minutes walking, 2 minutes resting) helped beta-blocker users improve endurance more than steady-state exercise. Try this: walk for 4 minutes, then stop and catch your breath for 2 minutes. Repeat five times. You’ll get more benefit in less time-and without pushing your heart too hard.
Red Flags: When to Stop and Call Your Doctor
Fatigue is normal. Danger isn’t.
- Resting heart rate below 45 bpm with dizziness or lightheadedness? This affects about 5% of users and needs medical review.
- Systolic blood pressure drops below 90 mmHg during exercise? This can signal cardiogenic shock and requires immediate care.
- Dry mouth and no sweat during mild activity? This happens in 12% of users and means you’re at risk of dehydration. Drink water-even if you don’t feel thirsty.
- Chest pain, fainting, or irregular heartbeat? Stop immediately and seek help.
These aren’t just warnings-they’re life-saving signs. If you notice any of these, don’t wait. Call your doctor or go to urgent care.

New Tools and Future Trends
The good news? Science is catching up. Newer beta-blockers like nebivolol (Bystolic) cause less reduction in VO₂ max-about 8-10% less than older versions. That means better exercise tolerance. Also, the European Society of Cardiology now recommends personalized exercise plans based on cardiopulmonary exercise testing (CPET), a lab test that measures exactly how your body responds to activity. It’s becoming more common in cardiac rehab centers.
Even wearable tech is adapting. Apple Watch’s software version 9.1 (released September 2023) now includes beta-blocker-adjusted heart rate zones. It doesn’t replace professional advice, but it’s a step toward smarter, medication-aware fitness tracking.
Bottom Line: You Can Still Be Active
Being on beta-blockers doesn’t mean you have to sit still. It means you have to work smarter. Forget chasing heart rate numbers. Focus on how you feel. Use the talk test. Listen to your body. Extend your warm-ups. Lower your weights. Walk longer. You’ll still get the benefits-better circulation, lower blood pressure, improved mood, and stronger heart-without pushing yourself into danger. The goal isn’t to be the fastest or strongest. It’s to stay healthy, safe, and active for the long haul.
Can I still run on beta-blockers?
Yes, but not the way you used to. Your pace will likely slow down. A 5K that took you 25 minutes might now take 29 minutes-even if you feel like you're putting in the same effort. That’s normal. Use the talk test: if you can speak in full sentences without gasping, you're at the right intensity. Avoid sprinting or high-intensity intervals unless cleared by your doctor.
Why do I feel more tired on beta-blockers even when I'm not exercising?
Beta-blockers reduce your body’s ability to respond to adrenaline, which affects more than just your heart. This can lead to lower energy levels, slower metabolism, and even reduced motivation. It’s not laziness-it’s pharmacology. Try spreading out your day with short walks, light stretching, or standing more often. Even small movements help maintain energy.
Should I stop beta-blockers to exercise better?
Never stop or change your dose without talking to your doctor. Beta-blockers are prescribed for serious reasons-like preventing heart attacks or managing heart failure. The fatigue you feel is a side effect, not a reason to quit. Instead, adjust your exercise routine to match your body’s new limits. You’ll stay safer and healthier in the long run.
Is walking enough if I can’t do more intense exercise?
Yes, absolutely. Walking is one of the best exercises for people on beta-blockers. It’s low-impact, easy to control, and improves heart health without overloading your system. Aim for 30-40 minutes most days. Add hills or a weighted vest to increase intensity safely. Studies show consistent walking reduces blood pressure and improves endurance-even with beta-blockers.
What’s the best time of day to exercise on beta-blockers?
Late morning or early afternoon is often best. Blood pressure tends to be lower in the morning right after taking your dose, and your body hasn’t fully adjusted yet. Avoid exercising right after taking your pill. Wait at least 2-3 hours. Also, avoid extreme heat or cold-your body’s ability to regulate temperature can be affected.


Michaela Jorstad
February 19, 2026 AT 15:41Just wanted to say thank you for this. I’ve been on metoprolol for 3 years now, and I thought I was just getting old or lazy. Turns out, it’s the meds. I switched to the talk test last year, and suddenly, I could walk 45 minutes without feeling like I’d run a marathon. No more guilt. No more staring at my watch like it’s judging me. Just breathe. Just move. You’re doing great.
Chris Beeley
February 19, 2026 AT 23:10Let me tell you something, folks-this whole 'talk test' nonsense is a Band-Aid on a gunshot wound. You’re telling people to abandon objective metrics? That’s like telling a pilot to fly by gut feeling because their altimeter is 'broken.' The fact that beta-blockers reduce VO₂ max by 15% isn’t a suggestion to lower standards-it’s a call for scientific adaptation. Why not use CPET? Why not get a lab-grade cardiopulmonary stress test? The AHA’s 'talk test' is cute, but it’s not evidence-based medicine-it’s wellness culture repackaged as cardiac rehab. If you’re serious about health, you don’t guess. You measure. And if your doctor won’t order a CPET? Find a new one. Period.