What Diabetic Meal Planning Really Means
Diabetic meal planning isn’t about strict rules or cutting out all carbs. It’s about making smart choices that help your body manage blood sugar without leaving you hungry or frustrated. The goal? Keep your glucose levels steady-between 80 and 130 mg/dL before meals and under 180 mg/dL two hours after eating-so you avoid energy crashes, cravings, and long-term complications like nerve damage or heart disease.
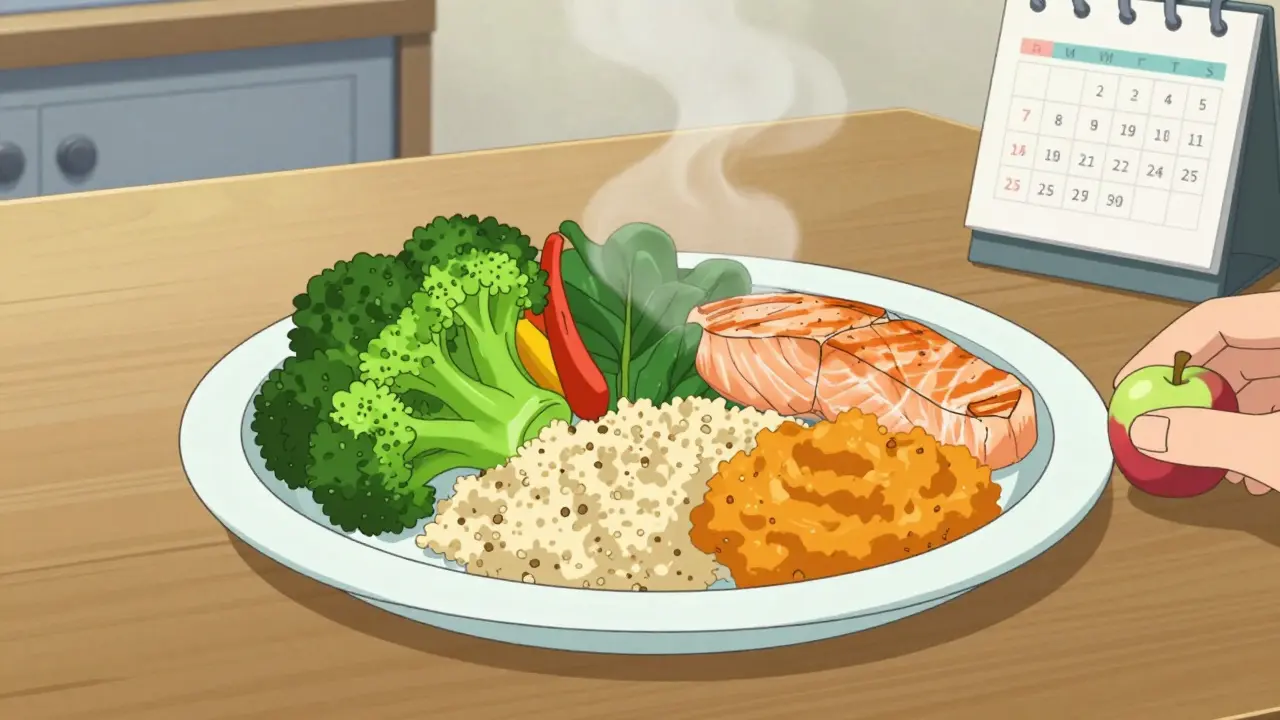
The American Diabetes Association (ADA) calls the Plate Method the easiest way to do this. No counting calories. No tracking carbs with apps. Just use a 9-inch plate-about the size of a standard business envelope-and divide it visually: half for non-starchy veggies, one-quarter for lean protein, and one-quarter for healthy carbs. That’s it. Studies show people who follow this method consistently lower their HbA1c by 0.3 to 2.0 percentage points over six months. That’s the difference between needing more medication and staying stable with diet alone.
Foods to Eat: Build Your Plate Right
Start with the biggest part of your plate: non-starchy vegetables. These are low in carbs and high in fiber, which slows digestion and keeps blood sugar from spiking. Think broccoli, spinach, kale, bell peppers, zucchini, mushrooms, asparagus, and green beans. Aim for 2.5 to 3 cups a day. You can eat them raw, steamed, roasted, or sautéed in olive oil-just skip the butter and creamy sauces.
Next, fill one-quarter of your plate with lean protein. This helps you feel full longer and doesn’t raise blood sugar. Good choices include skinless chicken breast, turkey, fish (especially salmon, mackerel, or sardines for omega-3s), tofu, eggs, and legumes like black beans and lentils. The CDC says 3 ounces of meat is about the size of your palm without fingers. Stick to that visual cue.
The last quarter? Carbs-but the right kind. Choose whole grains like quinoa, barley, and brown rice. Starchy vegetables like sweet potatoes and corn count here too. Even fruit belongs here: one small apple, a cup of berries, or a small orange. Avoid fruit juice-it’s sugar in liquid form with none of the fiber. The Mayo Clinic recommends eating fish at least twice a week. It’s not just good for your heart; it helps reduce inflammation linked to insulin resistance.
Healthy fats are your secret weapon. Add a tablespoon of olive oil to your salad, a quarter of an avocado to your sandwich, or a small handful of almonds as a snack. These fats slow down how fast carbs get absorbed, which means no sudden spikes. The Dietary Guidelines for Americans 2020-2025 say 25-35% of your daily calories should come from fats, with most of them being unsaturated. Skip the trans fats and limit saturated fats from fried foods and fatty cuts of meat.
Foods to Avoid: The Hidden Blood Sugar Triggers
Some foods sneak into your diet and wreck your blood sugar control-even if they seem healthy. White bread, white rice, and regular pasta are stripped of fiber and turn into sugar fast. Even whole wheat bread can spike glucose if it’s highly processed. Look for 100% whole grain, and check the ingredient list: if sugar is listed before the word “wheat,” it’s not a good choice.
Sugary drinks are the worst offenders. Soda, sweetened iced tea, fruit punch, and even some “vitamin waters” can contain 40 grams of sugar in one bottle-that’s more than a candy bar. A 2023 study in the Journal of the American Medical Association found that people who drank one sugary beverage daily had a 26% higher risk of developing Type 2 diabetes. Swap them for water, sparkling water with lemon, or unsweetened tea.
Processed meats like bacon, sausage, deli ham, and hot dogs are high in sodium and preservatives. The American Heart Association links them to increased insulin resistance and higher blood pressure. Even “low-fat” versions often replace fat with added sugar. Read labels. If a product says “fat-free” but has more than 5 grams of sugar per serving, it’s not your friend.
Don’t forget about flavored yogurts, granola bars, and breakfast cereals. Many are loaded with sugar under names like high-fructose corn syrup, dextrose, or cane juice. A single cup of fruit-flavored yogurt can have 20+ grams of sugar-equivalent to five teaspoons. Choose plain Greek yogurt and add your own berries instead.
And while it’s tempting to reach for “diabetic-friendly” snacks, many are just as processed as regular ones. They often contain sugar alcohols or artificial sweeteners that can still trigger cravings or digestive issues. Stick to whole, unprocessed foods as much as possible.

How to Eat When You’re Out or in a Rush
Meal planning doesn’t end when you leave home. Eating out is one of the biggest challenges. At restaurants, ask for your plate to be divided like the ADA recommends: half veggies, quarter protein, quarter carbs. Most places will accommodate if you ask. Order grilled or baked proteins, steamed veggies, and brown rice or quinoa instead of fries or white rice.
Fast food? It’s trickier, but doable. Skip the combo meals. Go for a grilled chicken sandwich without the bun (ask for it in a lettuce wrap), side salad with oil and vinegar, and a bottle of water. Avoid sauces-many are full of hidden sugar. At Mexican restaurants, choose fajitas with extra veggies and skip the rice and beans, or get a taco salad with lean meat and no shell.
Meal prep helps. Cook a big batch of quinoa and roasted veggies on Sunday. Portion out grilled chicken or tofu for the week. Keep hard-boiled eggs, nuts, and cut-up veggies in the fridge. When you’re hungry and tired, you’ll grab the healthy stuff instead of ordering pizza.
Timing Matters More Than You Think
It’s not just what you eat-it’s when. Eating at regular times helps your body predict when insulin will be needed. The ADA recommends spacing meals 2-3 hours apart. Skipping meals or eating all your carbs in one sitting can cause wild swings in blood sugar.
For kids with Type 2 diabetes, three small meals and three snacks a day help with growth and energy. For adults, three balanced meals with one or two small snacks (like a handful of almonds or a piece of fruit) works best. Avoid late-night snacking unless you’re truly hungry. Eating close to bedtime can raise morning blood sugar levels.
Some people find intermittent fasting helpful, but it’s not for everyone. If you’re on insulin or certain medications, skipping meals can be dangerous. Always talk to your doctor before changing your eating schedule.
What About Carbs? Do You Have to Cut Them?
No. Carbs aren’t the enemy. The problem is the type and amount. The Dietary Guidelines say 50-60% of your daily calories should come from carbs-but they must be complex, fiber-rich ones. That means whole grains, legumes, fruits, and vegetables-not white bread or candy.
Low-carb diets can work for some people, especially in the short term. But long-term, the most sustainable approach is balance. The ADA doesn’t recommend one-size-fits-all diets. What works for a 55-year-old man with high blood pressure might not work for a 30-year-old woman trying to get pregnant. Your plan should fit your life, culture, and preferences.
If you’re unsure how many carbs you need, ask a registered dietitian. Many insurance plans cover medical nutrition therapy for diabetes. A professional can help you figure out your ideal carb range based on your activity level, medications, and blood sugar patterns.

Real Meals That Work
Here are three simple, real-world meals based on the Plate Method:
- Breakfast: Scrambled eggs with spinach and mushrooms, one slice of whole-grain toast, and half a grapefruit.
- Lunch: Grilled chicken salad with mixed greens, cherry tomatoes, cucumbers, avocado, and a light vinaigrette. Side of ½ cup cooked quinoa.
- Dinner: Baked salmon, roasted broccoli and carrots, and ½ cup sweet potato mash with cinnamon.
The Diabetes Food Hub, run by the ADA, offers free recipes and lets you build your own meal plan online. You can drag and drop meals into a weekly calendar and even save favorites. It’s a great tool if you’re just starting out.
What If You Can’t Afford Healthy Food?
Food insecurity affects about 23% of adults with diabetes, according to the ADA. Fresh veggies, lean proteins, and whole grains can feel expensive. But there are ways to make it work.
Buy frozen vegetables-they’re just as nutritious, often cheaper, and last longer. Canned beans (rinsed to remove sodium) are a budget-friendly protein. Eggs are one of the most affordable sources of high-quality protein. Buy chicken thighs instead of breasts-they’re cheaper and still lean if you remove the skin.
Check if your local food bank or community center offers free diabetes-friendly food boxes. Some programs even deliver fresh produce to low-income households. The CDC’s Diabetes Prevention Program now includes virtual nutrition coaching-many are free or low-cost through public health departments.
Final Thought: It’s About Progress, Not Perfection
You don’t have to eat perfectly to see results. One study in The Lancet showed that people who stuck to a structured eating plan for six months-even if they slipped up once or twice a week-still saw big drops in HbA1c. The key is consistency, not purity.
Start with one change: swap soda for water. Add one extra serving of veggies to dinner. Use the plate method for one meal a day. Build from there. Your body will thank you-not just with better blood sugar, but with more energy, better sleep, and fewer cravings.
Can I still eat fruit if I have diabetes?
Yes, absolutely. Fruit contains natural sugars, but it also has fiber, vitamins, and antioxidants that help slow sugar absorption. Stick to whole fruits like apples, berries, oranges, and pears. Avoid fruit juice and dried fruit, which are concentrated in sugar. One serving is about one small piece or ½ cup chopped. Pair it with a handful of nuts to balance the impact on blood sugar.
Are artificial sweeteners safe for people with diabetes?
Most artificial sweeteners like stevia, sucralose, and aspartame don’t raise blood sugar directly. But they can still trigger cravings for sweet foods in some people. Some studies suggest they may affect gut bacteria in ways that influence insulin sensitivity over time. Use them sparingly. Water, unsweetened tea, or sparkling water with lemon are better long-term choices.
Should I count carbs or just use the plate method?
The plate method is great for beginners and works well for most people. If you’re on insulin or have trouble controlling blood sugar, carb counting gives you more precision. You can combine both: use the plate as your guide, then check labels to estimate carbs in your meals. Many apps let you scan barcodes to get carb counts quickly. Talk to your doctor or dietitian about what’s right for you.
Can I drink alcohol with diabetes?
Moderate alcohol can be okay-up to one drink per day for women and two for men. But alcohol can cause low blood sugar, especially if you’re on insulin or certain pills. Always drink with food, never on an empty stomach. Avoid sugary mixers like soda or juice. Stick to wine, light beer, or spirits with soda water and lime. Check your blood sugar before bed if you drink, as alcohol can cause delayed lows.
How long until I see results from changing my diet?
Some people notice better energy and fewer cravings within a week. Blood sugar levels often improve in 2-4 weeks. HbA1c, which shows your average blood sugar over 3 months, typically drops after 3-6 months of consistent changes. The key is sticking with it. Even small, steady improvements add up over time.

Skye Kooyman
January 26, 2026 AT 11:27Nicholas Miter
January 26, 2026 AT 12:49Aurelie L.
January 28, 2026 AT 04:50Robin Van Emous
January 29, 2026 AT 08:15Josh josh
January 29, 2026 AT 13:46Ashley Karanja
January 31, 2026 AT 04:06Geoff Miskinis
February 1, 2026 AT 11:07Betty Bomber
February 1, 2026 AT 13:09Simran Kaur
February 1, 2026 AT 18:11John Wippler
February 2, 2026 AT 14:16SWAPNIL SIDAM
February 3, 2026 AT 12:39Sally Dalton
February 3, 2026 AT 19:28Kipper Pickens
February 4, 2026 AT 11:01bella nash
February 6, 2026 AT 06:04