Every time you put on your watch, wash your hands, or apply lotion, your skin could be reacting to something invisible. If you’ve had a stubborn rash that won’t go away-itchy, red, flaky, sometimes oozing-you might have contact dermatitis. It’s not contagious. It’s not just dry skin. It’s your immune system overreacting to a chemical it thinks is dangerous. And the worst part? You probably don’t even know what’s causing it.
What Exactly Is Contact Dermatitis?
Contact dermatitis isn’t one thing. It’s two. There’s irritant contact dermatitis, which happens when something harsh like bleach or detergent burns your skin. But the kind that keeps coming back, the kind that makes you question every product you touch? That’s allergic contact dermatitis (ACD). It’s a delayed reaction-your skin doesn’t break out right away. It takes 24 to 72 hours. That’s why people think, “I didn’t touch anything new,” when really, they’ve been exposed to the same thing for months.
ACD happens when tiny chemicals, called haptens, slip through your skin’s barrier and latch onto proteins. Your body sees them as invaders. Langerhans cells-your skin’s immune sentinels-pick them up and send a signal to your lymph nodes. T-cells get activated. Days later, your skin erupts. It’s not an allergy like pollen or peanuts. It’s a slow-burn war inside your skin.
One in seven people tested for allergies has nickel sensitivity. That’s 17.4% of women and 3% of men in North America. And nickel isn’t just in jewelry. It’s in zippers, buttons, phone cases, eyeglass frames, even some coins. If you’re a woman who wears cheap earrings or a man who keeps his phone in his pocket, you’re at risk.
How Do You Find Out What’s Causing It?
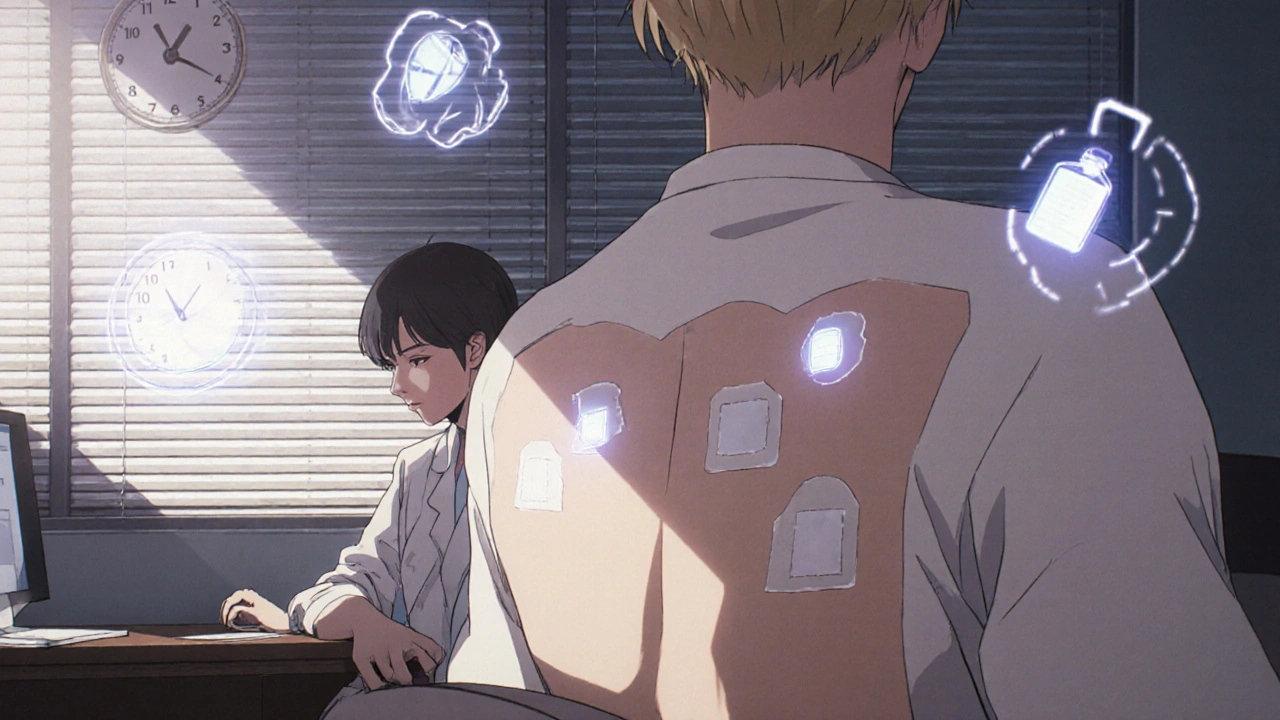
Guessing doesn’t work. You can’t just stop using everything and hope. That’s why patch testing is the gold standard. It’s not a prick test. It’s not a blood test. It’s a slow, deliberate process that sticks small patches of potential allergens to your back for two full days.
The standard test-called the TRUE Test-uses 29 common allergens. It’s done over three visits: Monday, Wednesday, Friday. On Monday, patches go on. You can’t get them wet. No sweating. No scratching. On Wednesday, they’re removed. The doctor checks for redness or bumps. Then you wait until Friday for the final read. That’s when the delayed reaction shows up.
The most common triggers found? Nickel sulfate (14.7% of positive cases), cobalt chloride (4.8%), thimerosal (5%), fragrance mix (3.4%), and balsam of Peru (3%). But here’s the problem: there are thousands of chemicals in everyday products. The TRUE Test only covers 29. If your rash keeps coming back, you might need expanded testing-up to 100 allergens. Hairdressers, nurses, construction workers: they often need this deeper panel because their jobs expose them to more chemicals.
Some people get false negatives. One Reddit user, ‘RashQueen2023,’ spent $350 out-of-pocket on a second round of testing because the first one missed formaldehyde. That’s why experts say: if your rash doesn’t improve after avoiding the obvious suspects, go back. Don’t give up.
What Are the Real Culprits? Beyond Nickel and Fragrance
People think fragrance means perfume. But fragrance mix is a blend of 8 common scent chemicals used in everything from shampoo to laundry detergent. Even “unscented” products can hide fragrance ingredients to mask other smells. And if you’re allergic to balsam of Peru, you might react to cinnamon, vanilla, citrus peels, or even some teas and wines.
Another sneaky one: cocamidopropyl betaine. It’s in shampoos, face washes, baby wipes. One patient, ‘EczemaWarrior87,’ had hand dermatitis for five years-until patch testing found it. Eliminate that one ingredient, and the rash vanished.
Then there’s formaldehyde. Used as a preservative in cosmetics, nail polish, and even some shampoos. It’s also released by other chemicals like quaternium-15 and DMDM hydantoin. You won’t see “formaldehyde” on the label. You’ll see these sneaky names. That’s why just reading labels isn’t enough-you need to know what to look for.
And don’t forget about rubber. Latex gloves? They’re not the only problem. Chemicals used in rubber manufacturing, like mercaptobenzothiazole, are common allergens for mechanics, healthcare workers, and even people who wear elastic waistbands.
How to Avoid Allergens Once You Know Them
Knowing your trigger is only half the battle. Avoiding it is the other half. And it’s harder than it sounds.
Start with the basics: ditch the cheap jewelry. Swap metal watches for silicone or plastic bands. Use a phone case made of silicone or fabric, not metal. Choose stainless steel over nickel-plated hardware.
For skincare, look for products labeled “fragrance-free,” not “unscented.” Fragrance-free means no added scent. Unscented can still contain masking agents. Check the ingredient list for “parfum,” “fragrance,” or “essential oils.” Avoid anything with balsam of Peru if you’re sensitive.
The American Contact Dermatitis Society created the Contact Allergen Replacement Database (CARD). It’s a free tool that tells you which products are safe based on your allergens. It lists over 18,000 products-from hand soap to sunscreen-that don’t contain your triggers. You don’t have to guess anymore.
For work-related exposure, talk to your employer. Hairdressers might need to switch to formaldehyde-free hair straighteners. Nurses might need non-latex gloves. OSHA requires employers to help identify workplace allergens. You have a right to a safe environment.
And patience matters. After avoiding your allergen, give it 2 to 4 weeks to heal. Studies show 68% of people see improvement in that window. Don’t rush. Don’t test it by using the product again. Let your skin recover.
Why Patch Testing Works-And Why It’s Not Perfect
Patch testing isn’t just a procedure. It’s a life-changing tool. Dr. Matthew Zirwas, a leading dermatologist, says it changes management in 60-70% of cases. That means people stop getting rashes. They stop buying new creams. They stop feeling anxious about every new product.
But it’s not flawless. Inter-observer variability can be as high as 30% if the doctor isn’t trained in contact dermatitis. That’s why you need to see a specialist-not just any dermatologist. Look for someone who does patch testing regularly. Ask how many tests they do a month.
Also, the test only tells you what you’ve been exposed to. If you haven’t touched a certain chemical in years, your body might not react anymore. That’s called tolerance. It’s rare, but it happens. And if you’ve been using a product for years without a reaction, and suddenly you develop one? That’s called sensitization. Your immune system changed its mind.
And yes, some allergens still slip through. That’s why experts are working on new methods. Blood tests measuring IL-18 levels are showing promise. One 2024 study found it correlates strongly with rash severity. Molecular diagnostics are coming. But right now? Patch testing is still the only way to know for sure.
What’s Changing in the World of Allergen Testing
The EU banned 26 fragrance allergens in cosmetics in 2003. The U.S. hasn’t done the same. The Safe Cosmetics Act has been stuck in Congress since 2021. That means American consumers are still exposed to chemicals banned in Europe.
By 2027, the EU will fully phase out guinea pig testing for chemical safety. The U.S. is moving toward non-animal methods, too. And by Q3 2025, the TRUE Test will expand from 29 to 80 allergens, adding new ones like those found in touchscreens and green cosmetics.
Meanwhile, companies are starting to label more clearly. Some brands now list allergens upfront. But it’s not mandatory. So you still have to read carefully.
Real Stories, Real Results
A 2023 survey of 1,247 people with contact dermatitis found that 82% improved after avoiding their allergens. And 76% said knowing the exact cause reduced their anxiety. That’s huge. For years, they blamed stress, diet, or bad luck. Turns out, it was their phone case.
One woman in Perth stopped getting rashes on her neck after switching from a stainless steel necklace to titanium. A construction worker stopped getting hand eczema after switching to nitrile gloves instead of latex. A teenager’s facial breakout cleared up after ditching a “natural” face wash that contained tea tree oil-something she thought was safe.
These aren’t rare cases. They’re common. And they all started with one question: “What am I touching?”
What to Do Next
If you’ve had a rash for more than two weeks that doesn’t respond to moisturizers or hydrocortisone:
- Stop assuming it’s eczema or dry skin.
- Write down everything you touch daily-soaps, lotions, jewelry, tools, gloves, even your laptop.
- Make an appointment with a dermatologist who does patch testing. Ask: “Do you use the TRUE Test? Do you offer expanded panels?”
- Don’t wait. The longer you’re exposed, the worse your skin gets.
- Once you know your allergen, use the CARD database to find safe products.
- Give your skin 4 weeks to heal. No cheating.
It’s not about being perfect. It’s about being informed. You don’t have to throw out everything. Just the things that are hurting you.
Can contact dermatitis go away on its own?
It can, but only if you stop touching the allergen. If you keep using the product or wearing the item that triggers it, the rash will keep coming back. Avoidance is the only cure. Moisturizers and creams help with symptoms, but they don’t fix the root cause.
Is patch testing painful?
No. The patches are taped to your back and don’t break the skin. You might feel mild itching or burning when the reaction appears, but the test itself is not painful. The biggest challenge is avoiding water and sweat for 48 hours while the patches are on.
Can I do patch testing at home?
No. Home patch tests aren’t reliable or standardized. They can give false results, cause severe reactions, or miss your true allergen. Only trained dermatologists using FDA-approved panels like the TRUE Test should perform this test.
How long does it take to see results after avoiding an allergen?
Most people see improvement in 2 to 4 weeks. Some notice changes in just a few days. But full healing can take up to 6 weeks. Don’t reintroduce the allergen too soon. Let your skin recover completely.
Are natural or organic products safer?
Not necessarily. Many natural ingredients like tea tree oil, lanolin, balsam of Peru, and essential oils are common allergens. “Organic” doesn’t mean hypoallergenic. Always check ingredient lists-even on natural brands.
Can I still wear jewelry if I’m allergic to nickel?
Yes-but only if it’s nickel-free. Look for jewelry labeled “hypoallergenic,” “surgical steel,” “titanium,” or “sterling silver (925).” Avoid plated jewelry; the coating wears off. You can also coat the inside of rings with clear nail polish as a temporary barrier.
Is contact dermatitis the same as eczema?
No. Eczema (atopic dermatitis) is an internal immune condition often linked to genetics and dry skin. Contact dermatitis is caused by direct contact with a specific chemical. You can have both. But they need different treatments. Patch testing helps tell them apart.
What if my patch test is negative but I still have a rash?
You might have irritant contact dermatitis, which doesn’t show up on patch tests. Or your allergen wasn’t in the test panel. Ask your doctor about expanded testing or a detailed exposure history. Sometimes, a chemical in a product is hidden under a vague name like “fragrance” or “preservative.”


Nikki C
November 24, 2025 AT 05:44I had a rash for two years thought it was eczema until I switched phone cases and it vanished overnight. My phone had a nickel-plated frame. Never even thought about it.
Jacob McConaghy
November 24, 2025 AT 22:18People act like this is some new fad but my grandma had this in the 70s and no one knew why. Patch testing was a joke back then. Now we got the tools, we just gotta use them. Stop blaming stress. It’s your damn watch.
Victoria Stanley
November 25, 2025 AT 22:27Just want to add that CARD database is a game changer. I used it when I found out I was allergic to cocamidopropyl betaine. Found 12 safe shampoos in 5 minutes. No more guessing. No more burning hands. Life changed.
akhilesh jha
November 27, 2025 AT 15:15In India, we use henna for weddings and skin decoration. Many don’t realize it often contains para-phenylenediamine - a known allergen. My cousin got severe blisters after a festival. Patch test later confirmed it. This isn’t just a Western problem.
Vineeta Puri
November 28, 2025 AT 11:19Thank you for this comprehensive guide. As a nurse who developed hand dermatitis from latex gloves, I can confirm that occupational exposure is severely under-discussed. Employers must be held accountable. We deserve safe working conditions - and patch testing should be offered as part of routine occupational health screening.
Jeff Hicken
November 30, 2025 AT 05:14so like… i stopped using all my stuff and now i just rub my face with butter? is that a thing? my dermatologist said no but i think its working? maybe?
Andy Louis-Charles
December 1, 2025 AT 21:28Also - if you’re allergic to balsam of Peru, avoid cinnamon rolls 🥮. I learned the hard way. Also tea, vanilla ice cream, and that ‘natural’ lip balm you think is harmless. Your skin is not a lab rat.
Natashia Luu
December 1, 2025 AT 22:27It is deeply irresponsible to suggest that ‘fragrance-free’ is safe. The FDA allows companies to hide dozens of allergens under that term. This is corporate deception disguised as consumer care. You are being manipulated. Your skin is the battlefield. Wake up.
Douglas cardoza
December 2, 2025 AT 18:21my sister got a rash from her yoga mat. yea. the rubber backing. no joke. switched to a cotton one and poof. gone. who knew?
Alex Dubrovin
December 2, 2025 AT 21:27My dad’s been wearing the same stainless steel watch for 15 years. Then one day, his wrist turns red. Turns out the clasp was nickel-plated. He didn’t even know it was plated. Just thought it was ‘cheap metal.’ Now he wears a silicone strap. No more rashes. No drama. Just peace.