Cephalosporin Cross-Reactivity Risk Calculator
This tool calculates the actual cross-reactivity risk between penicillin and cephalosporin antibiotics based on the latest medical research. The old 10% rule is outdated—our understanding of penicillin allergy and cephalosporin cross-reactivity has evolved significantly.
Many people believe that if they’re allergic to penicillin, they can’t take cephalosporins. That idea has been around for decades. But here’s the truth: cephalosporin allergy and penicillin cross-reactivity aren’t as simple as most doctors and patients think. The old 10% cross-reactivity rule? It’s outdated. In fact, it’s often wrong-and it’s leading to unnecessary risks, higher costs, and worse outcomes for patients.
Why the 10% Rule Is Outdated
For years, medical guidelines warned that if you’re allergic to penicillin, you have a 10% chance of reacting to cephalosporins. That number came from studies in the 1960s and 70s. But those studies were flawed. Back then, cephalosporin drugs were often contaminated with tiny amounts of penicillin because of how they were made. So when patients had reactions, it wasn’t because cephalosporins were similar to penicillin-it was because they were mixed with it.Today’s cephalosporins are pure. No contamination. And modern research shows the real cross-reactivity rate is much lower. Studies from the 2000s onward, including data from the CDC and Medsafe, now estimate cross-reactivity at just 2% to 5% for first- and second-generation cephalosporins. For third- and fourth-generation ones like ceftriaxone or cefepime? It’s less than 1%. That’s not a 1 in 10 chance. That’s closer to 1 in 100.
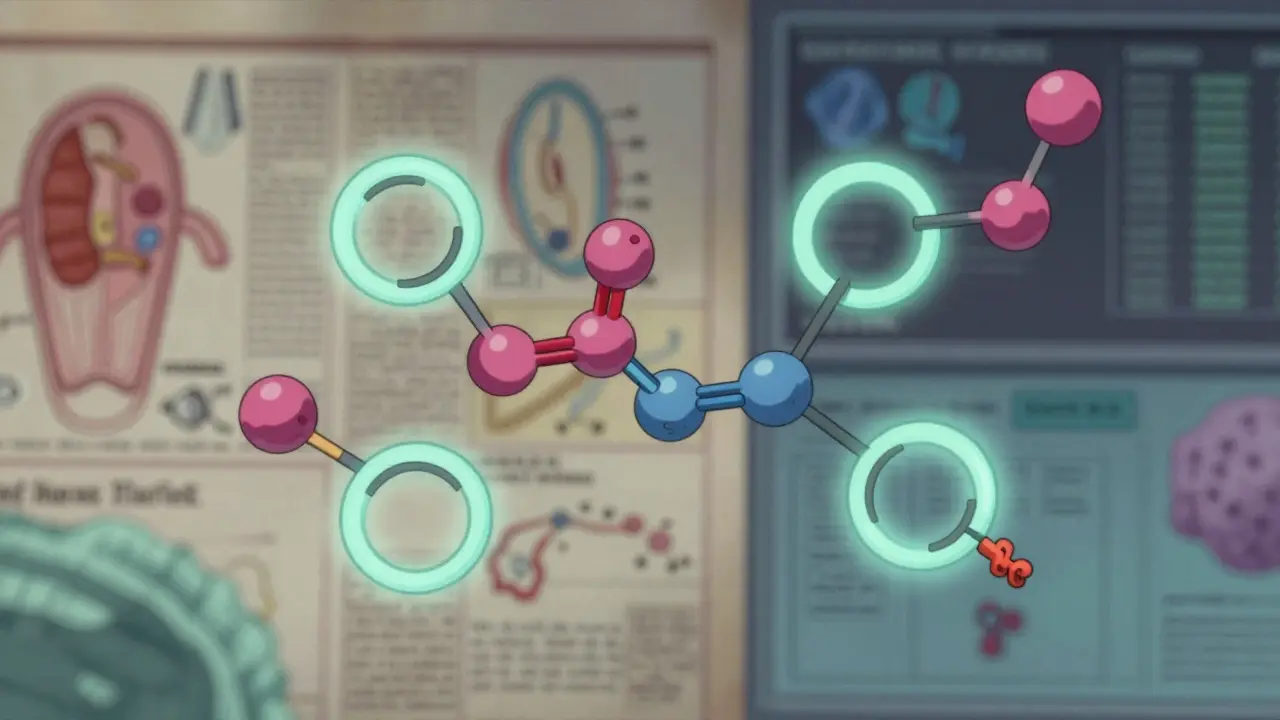
It’s Not the Ring-It’s the Side Chain
Penicillins and cephalosporins both have a beta-lactam ring. That’s the part people used to blame for cross-reactivity. But that’s not what triggers most allergic reactions. The real culprit? The side chains-the chemical groups attached to the core structure.Think of it like a lock and key. Your immune system doesn’t see the whole antibiotic. It sees specific shapes on the surface. If the side chain on a cephalosporin looks a lot like the side chain on the penicillin you reacted to, that’s when trouble can happen. For example, if you had an allergic reaction to amoxicillin, you might be at slightly higher risk for cefdinir or cefaclor, because they share similar side chains. But ceftriaxone? Its side chain is completely different. So even if you’re allergic to penicillin, ceftriaxone is very likely safe.
Research shows that side chains account for 42% to 92% of allergic reactions to penicillins. That’s why the old idea of “all beta-lactams are the same” is misleading. It’s not about the class-it’s about the structure.
Generations Matter-A Lot
Cephalosporins come in five generations. Each one has different side chains and different levels of risk if you have a penicillin allergy.- First-generation (like cefazolin, cephalexin): Highest risk. Similar side chains to penicillin G and ampicillin. Cross-reactivity around 2-8%.
- Second-generation (like cefuroxime, cefaclor): Moderate risk. Some overlap with amoxicillin. Cross-reactivity around 2-5%.
- Third-generation (like ceftriaxone, cefixime): Very low risk. Different side chains. Cross-reactivity under 1%.
- Fourth-generation (like cefepime): Also very low risk. Even more structurally distinct.
- Newer agents (like ceftolozane/tazobactam): Not classified in traditional generations. No clear data yet, but side chains are unique. Likely safe.
Here’s the key takeaway: If you need a cephalosporin, avoid first-generation unless there’s no other option. Third-generation drugs like ceftriaxone are often the safest choice-even for people with confirmed penicillin allergies.
Anaphylaxis Is Extremely Rare
One of the biggest fears is anaphylaxis-a life-threatening reaction. But data from large patient studies shows how rare it really is.The Kaiser Permanente study followed over 3,300 patients who said they were allergic to cephalosporins. They were given cephalosporins anyway-mostly first-generation. Result? Zero cases of anaphylaxis. Not one.
The CDC estimates that anaphylaxis from cephalosporins in penicillin-allergic patients happens in only 1 out of every 52,000 people. That’s less likely than being struck by lightning. Most reactions people report are rashes or stomach upset-not true allergies. Many are just intolerances or coincidental reactions.
What About Penicillin Allergy Testing?
If you’ve been told you’re allergic to penicillin, you might not actually be. Studies show that 90% to 95% of people who say they have a penicillin allergy can safely take it after proper testing.Penicillin skin testing is the gold standard. It involves a small prick with penicillin and its breakdown products. If it’s negative, you’re almost certainly not allergic. Many hospitals now have allergy programs that test patients before surgery or hospital admission. If you’ve been labeled “penicillin allergic” for years, ask your doctor about testing. It could open up safer, cheaper, more effective treatment options.
Even if you’re not tested, guidelines from the CDC and Infectious Diseases Society of America say third-generation cephalosporins can be used safely in patients with a history of penicillin allergy-unless they had a true IgE-mediated reaction like anaphylaxis, hives, or swelling within the last 10 years.
Why This Matters for Your Health
When doctors avoid cephalosporins because of outdated fears, they turn to other antibiotics. Fluoroquinolones. Clindamycin. Vancomycin. These drugs are broader-spectrum. They kill more types of bacteria-including the good ones.This leads to problems:
- Higher rates of Clostridioides difficile infections (C. diff), which cause severe diarrhea and can be deadly.
- More antibiotic resistance, making future infections harder to treat.
- Longer hospital stays and higher costs. The CDC estimates billions of dollars are wasted each year because of unnecessary antibiotic choices.
Using the right antibiotic isn’t just about avoiding allergies. It’s about using the most targeted, least harmful option. Cephalosporins are often that choice. Especially third-generation ones.
What Should You Do?
If you’ve been told you’re allergic to penicillin:- Don’t automatically avoid cephalosporins-especially third-generation ones like ceftriaxone.
- Ask your doctor if you’ve ever had a true allergic reaction (hives, swelling, trouble breathing) or just a rash or upset stomach.
- Request penicillin skin testing if you’re going to need antibiotics often (like for surgery or recurrent infections).
- If you need a cephalosporin, ask which one is best based on your history. Avoid first-generation unless absolutely necessary.
- Don’t assume a reaction to one cephalosporin means you can’t take any. If the side chains are different, you may still be safe.
And if you’re a healthcare provider: Stop using the 10% rule. Update your prescribing habits. Use the latest guidelines. Your patients will get better care-and fewer side effects.
What’s Next?
The medical community is slowly catching up. Hospitals are launching penicillin allergy delabeling programs. Electronic health records are being updated to flag when a patient’s allergy might be mislabeled. More research is focusing on identifying exact side-chain patterns to predict reactions with even greater accuracy.But change moves slowly. The FDA still lists a 10% cross-reactivity warning on cephalosporin labels. That’s based on 1970s data. Meanwhile, the CDC, Medsafe, and top allergy societies have moved on. The gap between guidelines and labels is causing confusion-and harm.
The message is clear: Don’t let old myths keep you from safe, effective treatment. Cephalosporins aren’t dangerous just because you’re allergic to penicillin. The science says otherwise.
Is it safe to take ceftriaxone if I’m allergic to penicillin?
Yes, for most people. Third-generation cephalosporins like ceftriaxone have a cross-reactivity rate of less than 1% with penicillin-allergic patients. The risk is extremely low, especially if your penicillin reaction wasn’t severe (like anaphylaxis). Many guidelines now consider ceftriaxone safe to use in patients with penicillin allergy, unless they had a life-threatening reaction within the last 10 years.
Can I be allergic to cephalosporins even if I’m not allergic to penicillin?
Yes. About 1% to 3% of people develop allergic reactions to cephalosporins even without any history of penicillin allergy. This is because the immune system can react to the drug’s unique side chains or other components. So, no penicillin allergy doesn’t mean you’re guaranteed to be safe with cephalosporins-but your risk is still low.
Why do some doctors still avoid all cephalosporins for penicillin-allergic patients?
Because many providers still rely on outdated information. Studies show 80% to 90% of doctors believe the old 10% cross-reactivity myth. Drug labels haven’t caught up, and medical training often hasn’t been updated. It’s a case of inertia-until testing becomes routine, many will continue to avoid cephalosporins out of caution, even when the science says it’s unnecessary.
What’s the difference between a penicillin allergy and intolerance?
A true penicillin allergy involves the immune system-symptoms like hives, swelling, wheezing, or anaphylaxis. An intolerance is a side effect that doesn’t involve the immune system-like nausea, diarrhea, or a mild rash. Many people call a stomach upset an “allergy,” but it’s not the same thing. Only immune-mediated reactions predict cross-reactivity with cephalosporins.
Should I get tested for penicillin allergy?
If you’ve been told you’re allergic to penicillin and you might need antibiotics in the future (for surgery, infections, or chronic conditions), yes. Skin testing is safe, quick, and accurate. If the test is negative, you can safely use penicillin and most cephalosporins. This reduces your risk of side effects from broader-spectrum antibiotics and saves money in the long run.

Harshit Kansal
January 5, 2026 AT 19:28Man, I had a rash after amoxicillin in 2015 and they’ve been treating me like I’m gonna drop dead if I so much as smell a cephalosporin. This post just blew my mind. I’ve been avoiding ceftriaxone like it’s poison when I probably could’ve had it five years ago.
Jeane Hendrix
January 7, 2026 AT 18:23So let me get this straight-the cross-reactivity isn’t about the beta-lactam ring, it’s about the side chains? That’s wild. I’ve been reading all these papers on immunoglobulin E binding motifs and it’s like, ohhhhh so that’s why cefdinir tripped me but cefepime didn’t. The structural biology here is actually kind of beautiful if you think about it. Also, typo: ‘side chian’ in my notes lol.
Katie Schoen
January 9, 2026 AT 08:55So doctors are still using a 1970s rule because the FDA label hasn’t updated? That’s like refusing to use GPS because your car manual says to use a paper map. I’m not mad, I’m just disappointed.
Saylor Frye
January 10, 2026 AT 06:10It’s fascinating how medical dogma persists despite overwhelming evidence. The 10% myth is a textbook case of cognitive inertia in clinical practice. I’ve seen residents refuse ceftriaxone for MRSA prophylaxis because of a 15-year-old penicillin rash-when clindamycin is literally worse on every metric. This isn’t just outdated, it’s unethical.
Molly McLane
January 11, 2026 AT 06:31I’m a nurse in a busy ER and I’ve seen this firsthand. Patients come in with ‘penicillin allergy’ written in their chart like it’s a death sentence. We’ve started doing quick allergy consults before surgery and the results? 9 out of 10 turn out to be non-allergic. It’s not just safer-it’s cheaper, faster, and less likely to give them C. diff. We’re starting a hospital-wide delabeling initiative next month. If you’ve been told you’re allergic, please get tested. You’re not being dramatic. You’re being misinformed.
Vinayak Naik
January 11, 2026 AT 12:30Bro this is gold. In India we still get cephalexin prescribed like it’s candy for every cold. But I had a cousin who broke out in hives after cefaclor and now she’s terrified of all antibiotics. Turns out her reaction was to the side chain of cefaclor, not penicillin. She’s now on ceftriaxone for pneumonia and doing fine. Side chains are the real MVPs here. Also, ‘cephalosporin’ is a mouthful, but worth it.
Gabrielle Panchev
January 12, 2026 AT 02:46Wait-so you’re telling me that the entire medical community has been basing prescribing decisions on a flawed statistic from the 1970s, when contamination was the actual problem, and now, with pure drugs, the real cross-reactivity rate is less than 1% for third-gen cephalosporins? And yet, hospitals still refuse to update their EHRs? And drug labels still say 10%? And this isn’t being shouted from the rooftops? This isn’t just negligence-it’s systemic malpractice. Why isn’t this on the front page of JAMA? Why isn’t the AMA issuing a statement? Why aren’t patients being notified? This is like telling people not to drink water because someone once drank contaminated water in 1952 and got sick. I’m not even mad-I’m just… stunned.
Katelyn Slack
January 14, 2026 AT 02:30my doc told me i was allergic to penicillin after a rash when i was 8. i just found out i can probly take ceftriaxone?? i think i need to ask about testing. thanks for this.
Melanie Clark
January 15, 2026 AT 14:24This is all part of the pharmaceutical agenda to push more expensive antibiotics. The CDC? Medsafe? They’re all funded by Big Pharma. Why would they want you to use cheap, safe cephalosporins when they can sell you vancomycin at $2,000 a dose? And don’t even get me started on how they’re erasing your allergy history to sell you more drugs. I’ve seen the data-it’s all fake. The real cross-reactivity is 87%. They just don’t want you to know.