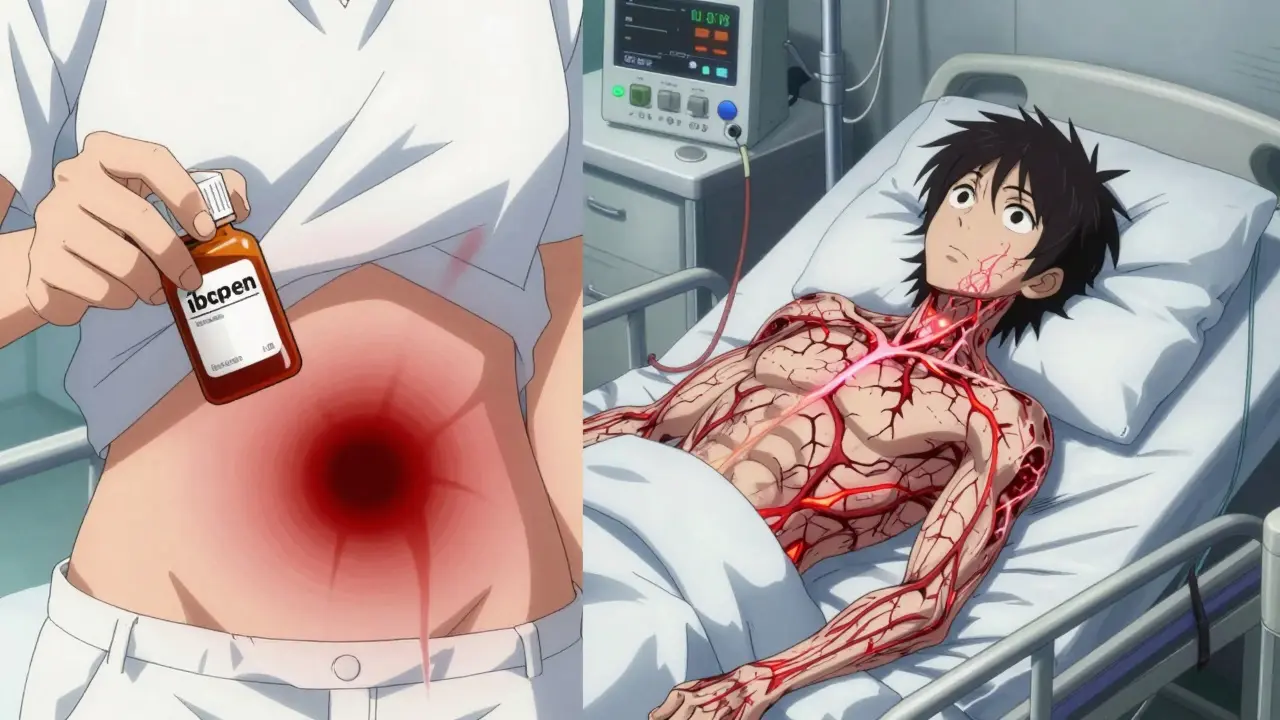
Combining blood thinners with common pain relievers like ibuprofen or naproxen isn’t just a bad idea-it’s a dangerous mix that can send you to the hospital, or worse. This isn’t theoretical. Real people, real data, and real bleeding events prove it. A 2024 study tracking over 51,000 patients on blood thinners found that taking NSAIDs more than doubled their risk of serious bleeding. And it’s not just stomach bleeding. It’s brain bleeds, lung bleeds, kidney bleeds-anywhere in the body.
What Happens When Blood Thinners and NSAIDs Meet?
Blood thinners work in one of two ways: they either stop your blood from clotting properly (anticoagulants like warfarin, rivaroxaban, or apixaban) or they prevent platelets from sticking together (antiplatelets like aspirin). NSAIDs-like ibuprofen, naproxen, and diclofenac-do something else entirely. They block enzymes called COX-1 and COX-2. COX-1 is especially important because it helps protect your stomach lining and keeps platelets working right. When NSAIDs shut down COX-1, your stomach gets more vulnerable to damage, and your platelets can’t clump together to stop bleeding.Now imagine both systems are down at once. Your blood thinners are already slowing clotting. Your NSAIDs are making your platelets sluggish and your stomach lining fragile. The result? A perfect storm for internal bleeding. This isn’t a rare side effect. It’s a predictable, well-documented outcome that shows up in hospital records across multiple countries.
Which NSAIDs Are the Most Dangerous?
Not all NSAIDs are created equal when it comes to bleeding risk. The 2024 Danish study broke it down clearly:- Naproxen: 4.1 times higher risk of hospitalization for bleeding
- Diclofenac: 3.3 times higher risk
- Ibuprofen: 1.79 times higher risk
Why the difference? It comes down to how strongly each drug blocks COX-1. Naproxen is the strongest COX-1 inhibitor of the three, which is why it’s the riskiest. Diclofenac is close behind. Ibuprofen is less potent, but still dangerous-especially if you take it daily or in high doses.
And no, switching to a "gentler" NSAID like celecoxib (a COX-2 inhibitor) doesn’t help. A 2019 study from the American College of Cardiology found that even selective COX-2 inhibitors still raised bleeding risk just as much as traditional NSAIDs when taken with blood thinners. The idea that "selective" means "safe" is a myth.
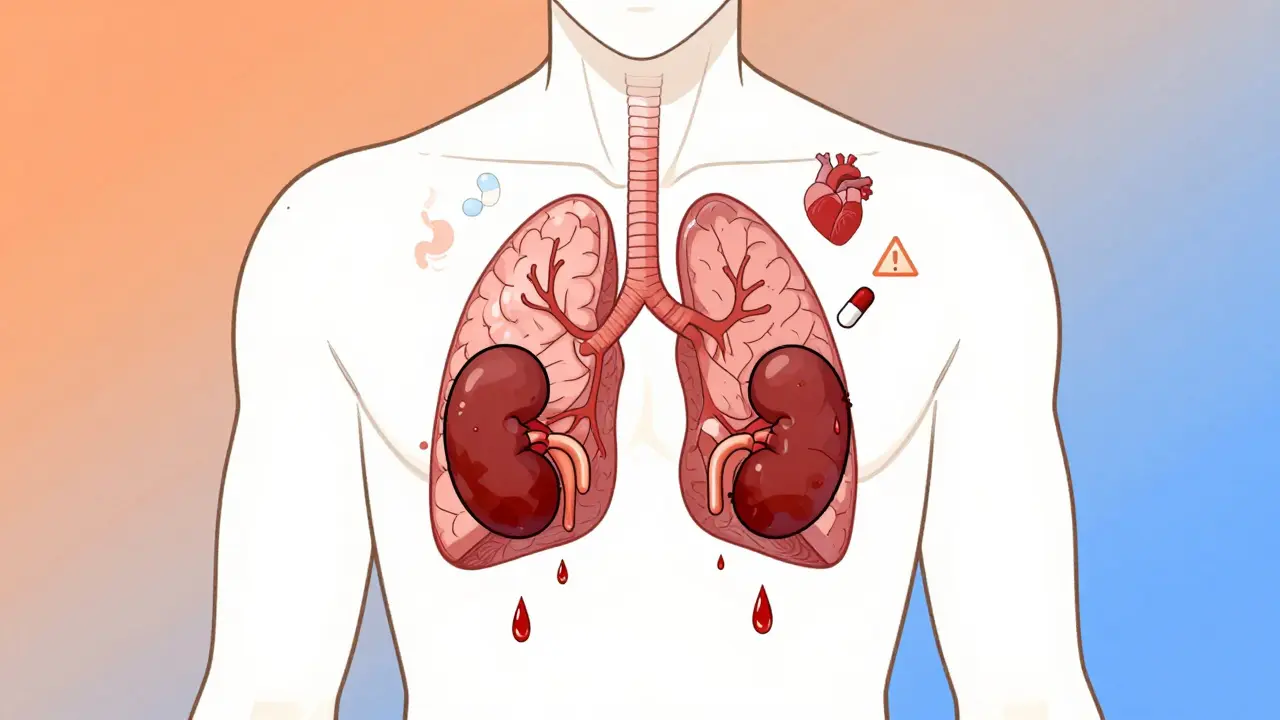
It’s Not Just Your Stomach at Risk
Most people think the danger is only stomach ulcers or bloody stools. That’s only part of the story. The same Danish study showed:- 2.24 times higher risk of gastrointestinal bleeding
- 3.22 times higher risk of bleeding in the brain
- 1.36 times higher risk of bleeding in the lungs
- 1.57 times higher risk of bleeding in the urinary tract
- Nearly three times higher risk of anemia from chronic blood loss
That’s the scary part. You might feel fine-no stomach pain, no black stools-yet still be bleeding internally. Brain bleeds can happen without warning. Lung bleeds can mimic pneumonia. Urinary bleeding might be mistaken for a UTI. And by the time symptoms show up, it’s often too late.

Does It Matter What Blood Thinner You’re On?
No. Whether you’re on warfarin, the old-school blood thinner, or one of the newer ones like apixaban (Eliquis), dabigatran (Pradaxa), or rivaroxaban (Xarelto)-the risk stays the same. A common misconception is that newer blood thinners are safer with NSAIDs. They’re not. The 2024 study confirmed that the bleeding risk jumped equally across all anticoagulant classes.That means if you’re on any blood thinner-prescribed for atrial fibrillation, a past blood clot, or a mechanical heart valve-you need to treat NSAIDs the same way: as a potential threat.
What Should You Take Instead?
If you’re on a blood thinner and need pain relief, acetaminophen (Tylenol) is your best bet. It doesn’t affect platelets or the stomach lining. It won’t raise your bleeding risk. It’s not perfect-it doesn’t reduce inflammation like NSAIDs-but for pain and fever, it’s safe and effective.For chronic pain, like arthritis, consider non-drug options:
- Physical therapy
- Heat or cold packs
- Weight management to reduce joint stress
- Topical creams with capsaicin or menthol
If you absolutely must use an NSAID-say, for a sudden gout flare or severe injury-use the lowest dose for the shortest time possible. Even a few days of use can raise your risk. And never take NSAIDs without talking to your doctor first.
Why Do People Keep Doing This?
Many patients don’t realize OTC painkillers are drugs. They think, "It’s just ibuprofen from the grocery store-it’s harmless." But if you’re on a blood thinner, that bottle of Advil is just as dangerous as a prescription pill.Doctors miss it too. In busy clinics, medication reviews often focus on prescriptions and skip OTCs. A 2020 study found that nearly half of patients on blood thinners who took NSAIDs never mentioned them to their provider. They didn’t think it mattered. It does.
And here’s the kicker: the more people take NSAIDs daily, the more this problem grows. In the U.S., over 30 billion OTC ibuprofen tablets are sold every year. Millions of people with atrial fibrillation or deep vein thrombosis are taking them without knowing the risk.
What Should You Do Right Now?
If you’re on a blood thinner:- Check your medicine cabinet. Do you have ibuprofen, naproxen, diclofenac, or aspirin? Even if you haven’t taken them in months, keep them out of reach.
- Look at your pharmacy list. Did your doctor prescribe any NSAID? Ask if it’s still necessary.
- Ask your pharmacist: "Is this safe with my blood thinner?" Don’t assume they know your full list-bring all your meds, including supplements.
- Switch to acetaminophen for pain. If it doesn’t help, talk to your doctor about alternatives.
- If you’ve had unexplained bruising, dark stools, dizziness, or fatigue lately-tell your doctor. It could be internal bleeding.
There’s no safe amount of NSAID use when you’re on a blood thinner. Not a pill a week. Not a single dose for a headache. The risk is real, measurable, and preventable.
What’s Being Done About It?
Health systems are starting to catch on. Some hospitals now use electronic alerts that flag when a doctor tries to prescribe an NSAID to someone on a blood thinner. Pharmacists are being trained to ask about OTC meds during refill checks. The American College of Cardiology now recommends "antithrombotic stewardship"-system-wide efforts to catch and stop these dangerous combinations before they cause harm.But until these systems are universal, the responsibility falls on you. Don’t wait for an alert. Don’t assume your doctor knows. Don’t think "it’s just one pill." Your blood doesn’t care if it’s prescription or over-the-counter. It only knows whether it can clot-or not.
Can I take aspirin if I’m on a blood thinner?
No. Aspirin is an NSAID and a powerful antiplatelet drug. Taking it with any blood thinner-warfarin, Eliquis, Xarelto, etc.-doubles your bleeding risk. Even low-dose aspirin for heart protection should only be used under strict medical supervision, and even then, it’s rarely combined with newer anticoagulants. Never start aspirin on your own if you’re on a blood thinner.
Is Tylenol (acetaminophen) really safe with blood thinners?
Yes, acetaminophen is the safest over-the-counter pain reliever for people on blood thinners. It doesn’t affect platelets or stomach lining. However, don’t exceed 3,000 mg per day, especially if you have liver disease or drink alcohol regularly. Always check with your doctor if you’re unsure about dosage.
What if I accidentally took ibuprofen with my blood thinner?
One dose is unlikely to cause immediate harm, but it still raises your risk. Stop taking it right away. Watch for signs of bleeding: unusual bruising, red or black stools, vomiting blood, severe headaches, dizziness, or shortness of breath. Call your doctor or go to urgent care if you notice any of these. Don’t wait for symptoms to get worse.
Can I use topical NSAIDs like Voltaren gel instead?
Topical NSAIDs like diclofenac gel are absorbed through the skin, so less enters your bloodstream. Studies suggest they carry a much lower bleeding risk than oral forms-but they’re not zero risk. If you’re on a strong blood thinner, talk to your doctor first. For mild joint pain, heat, ice, or physical therapy are safer bets.
Do I need to stop NSAIDs permanently?
If you’re on a blood thinner long-term-which most people are-yes. There’s no safe long-term use of NSAIDs with anticoagulants. Even occasional use adds up. For chronic pain, focus on non-drug options and acetaminophen. If your pain is so severe that you feel you need NSAIDs daily, talk to your doctor about underlying causes and alternative treatments, not just pain relief.
Why do doctors still prescribe NSAIDs to people on blood thinners?
Sometimes they don’t know the patient is on a blood thinner. Other times, they assume the patient isn’t taking OTC meds. Some doctors think newer anticoagulants are safer with NSAIDs-this is false. The 2024 study proved otherwise. The best defense is you: always tell your doctor every medication you take, even if you think it’s "just OTC."

vishnu priyanka
January 13, 2026 AT 06:05Man, I just checked my cabinet and found three ibuprofen bottles I forgot about. Been on Eliquis for AFib since last year. Guess I’m switching to Tylenol from now on. Thanks for the wake-up call.
Angel Tiestos lopez
January 14, 2026 AT 08:47bro i took naproxen last week for my back 😭 i thought it was just "a little pain"... now i’m scared to even sneeze. why does life have to be this hard?? 🥲💊
Pankaj Singh
January 15, 2026 AT 09:05This is why people die from dumbass OTC choices. You think you’re being smart by popping Advil like candy? Wake up. This isn’t a blog-it’s a death sentence waiting to happen. Stop being lazy and get real.
Scottie Baker
January 17, 2026 AT 04:35I’m on Xarelto and I’ve been taking ibuprofen for my knee since 2020. I’m not gonna lie-I’m kinda freaking out right now. My wife just found my stash. She’s not talking to me. I think I’m gonna cry. 😭
Diana Campos Ortiz
January 19, 2026 AT 00:52I’m so glad someone finally laid this out clearly. I’ve been on warfarin for 8 years and never realized how dangerous OTC meds could be. I’ve already tossed my naproxen. Tylenol it is. Thank you for saving lives with this post.
Jesse Ibarra
January 19, 2026 AT 21:11Oh wow, another "medical expert" telling people what to do. Did you even read the study? Or just skim the headline like the rest of the sheeple? COX-2 inhibitors are totally fine if you’re careful. You’re fearmongering.
laura Drever
January 20, 2026 AT 03:31so like... tylenol is safe? ok cool. also i take aspirin daily for my heart. is that bad? 🤷♀️
Randall Little
January 21, 2026 AT 02:09Interesting how the study didn’t control for dosage duration or liver function. Also, acetaminophen has its own risks-liver toxicity, especially in alcohol users. You’re replacing one danger with another without acknowledging the trade-offs. This is lazy public health messaging.
jefferson fernandes
January 22, 2026 AT 00:04Listen. I’m a nurse. I’ve seen patients bleed out from this exact combo. I’ve held their hands while they lost 4 units of blood because they thought "it’s just one pill." Please, for the love of God-don’t be the person who says, "I didn’t know." You knew. You just didn’t care. Stop. Now. Switch to Tylenol. Call your doctor. Do it today.
Acacia Hendrix
January 22, 2026 AT 14:27While the COX-1 inhibition mechanism is well-documented, the clinical significance of bleeding risk in low-dose, intermittent NSAID use remains underpowered in the cited cohort. The hazard ratio of 4.1 for naproxen is statistically significant but not necessarily clinically actionable without stratification by renal function, age, and concomitant antiplatelet burden. A risk-benefit analysis is warranted.
sam abas
January 24, 2026 AT 00:17Okay, let’s be real here-this whole thing is a scare tactic. People have been taking ibuprofen with blood thinners for decades. Hospitals are full of people on warfarin who take Advil for headaches and they’re fine. The study? Overblown. 51,000 people? That’s nothing compared to the billions who’ve taken NSAIDs safely. Also, Tylenol is worse for your liver than NSAIDs are for your stomach. And what about people with arthritis who can’t move without naproxen? You just want them to suffer? Wake up. This isn’t medicine-it’s moral panic dressed up as science.
Angel Molano
January 25, 2026 AT 12:23You’re a murderer if you take NSAIDs on blood thinners. Stop. Now.
Vinaypriy Wane
January 26, 2026 AT 22:35Thank you so much for sharing this. I’ve been on Xarelto since my DVT, and my mom used to take naproxen for her arthritis. I just called her and made her throw it out. She cried. But she’s safe now. Please, everyone-tell your loved ones. This could save a life.